CALL TODAY 646-846-1136 | EMAIL
Surgery for Esophageal Cancer – General Surgeon NYC
Esophagus Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
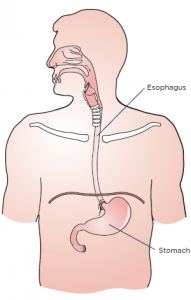
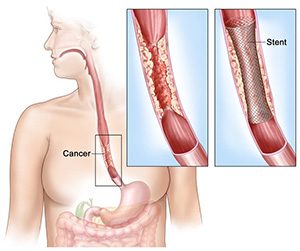
Esophagogastrectomy or esophagus surgery entails doing away with the entire esophagus (and often a stomach part) for treating esophageal cancer, Barrett’s esophagus, achalasia, esophageal stenosis, and GERD. The thoracic surgeon transforms the remaining section of the stomach into a tubular form serving as the replacement for the excised esophagus. The reconstructed esophagus enables the patient to swallow as he or she was doing before the surgery.
Steps
A surgical team comprising of medical specialists and headed by a thoracic or general surgeon performs esophagogastrectomy. The surgical procedure is usually open-type and is carried out in three separate ways.
- Transthoracic esophagectomy (TTE) is conducted via the chest cavity
- Transmittal esophagectomy (THE) is performed by making incisions in the breastbone and the neck’s left side
- En bloc esophagectomy is performed by perforating the abdomen, chest, and neck
Nowadays, the majority of the esophageal surgeries are done using the minimally-invasive laparoscopic procedure where 5-6 fine incisions are made in the abdomen, chest, and neck. The total number of slits (along with their locations) to be made are decided based on the purpose of carrying out the operation and whether the patient has undergone abdominal or thoracic surgeries on previous occasions.
Regardless of the type or method used, the operation is complex thereby necessitating an extended stay in the hospital. If the metastasis is limited to the esophagus and not spread further, excising the gullet and adjacent lymph nodes might help reverse cancer. Alas, most of the cases are detected at an advanced stage compelling the surgeon to go for a compound surgery.
Benefits
Minimally invasive esophagectomy has proven to be more effective compared to open esophagectomy as the postoperative mortality and morbidity rates related to the former are much lower. There are numerous studies to corroborate the outcomes associated with MIE are better than PE. Some of the likely benefits associated with MIE vis-à-vis PE comprise:
- Ashorter period of hospitalization
- Less painful procedure
- Reduced risk of complications or infections
- Less bleeding (and hence fewer transfusions)
- Speedier return to leading a normal life
Side Effects
Some complications related to esophageal surgery are common to other forms of surgery including but not limited to:
- Stroke and heart attack (while the operation is in progress)
- Shortness of breath
- Anastomotic leaking (low blood pressure, vomiting, surgical wound drainage, increased heart rate, and so on)
- Bleeding
- Pulmonary embolism
Complications or risks particularly associated with esophagogastrectomy (which are somewhat rare) include:
- Acute chest infection
- Pulmonary complications, particularly pneumonia
- An injury or wound to the adjacent organs during the operation
- Leakage at the junction of the conjoined stomach and esophagus
Precautions
The surgeon who will operate will spell out the risks about the surgery as well as the preparations and precautions you to need to take before, after and during the procedure. You’ll have to quit smoking altogether at least before the surgery and possibly afterward as well. You’ll have to abide by the instructions specified by your surgeon once you’re discharged from the hospital.
The precautions that you’ll need to take will revolve around your diets, medications, clothing, personal accessories, and lifestyle.
Prognosis
The quality of life of most patients improves post-surgery, but some complications linger on. Follow-up care in the form of pain management, lung therapy, psychosocial care, and nutritional evaluations are highly recommended by the medic to keep the complications or risks at bay.
Concluding Remarks
Minimally invasive esophagectomy or esophagogastrectomy is evidentially the best form of surgical treatment for patients with esophageal cancer. If you or somebody close to you has been diagnosed with neoplasm of the esophagus, you can contact us to make an appointment with our general surgeon for a consultation.
References
- https://www.uwhealth.org/healthfacts/surgery/4281.pdf
- https://www.cancer.org/cancer/esophagus-cancer/treating/surgery.html
- https://www.ariahealth.org/programs-and-services/surgery/general-surgery/surgery-for-esophagus
- https://www.cancercenter.com/esophageal-cancer/surgery/
- https://www.healthline.com/health/esophagectomy-open#postsurgery
- https://www.cancercenter.com/esophageal-cancer/da-vinci-surgical-system/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4283863/
- https://www.mayoclinic.org/tests-procedures/esophagectomy/about/pac-20385084
- https://www.uwhealth.org/healthfacts/surgery/4281.pdf
- https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=134&contentid=154

