CALL TODAY 646-846-1136 | EMAIL
Surgical Experts Dedicated to Improving Lives
At Lenox Hill Minimally Invasive Surgery PLLC, Dr. Valery Dronsky and his staff of medical professionals provide compassionate care with the highest ethical & professional standards. In our state of the art facility, we offer surgical services using only the most cutting edge and current procedures and treatments. We specialize in general surgery, including extensive experience in performing hernia repair surgery. Our expertise is in minimally invasive surgery and robotic surgery. Minimally invasive and robotic surgery often allow patients to experience easier recovery than traditional open surgery. They also allow for more precise and less traumatic surgery. When robotic and minimally invasive surgery is not an option, we are also skilled and experienced in traditional open surgical procedures.
Dr. Dronsky is an experienced and highly skilled surgeon having undergone extensive training in school, residency and fellowships. He practices medicine with ethical behavior, compassion and superb bedside manner. In the operating room he exhibits precision mechanical abilities, analytical thinking and the ability to visualize tissue in three dimensions. These innate and learned skills allow Dr. Dronsky to be one of the most dexterous and skilled professionals in New York City and the Country.
Call us: 646-846-1136
PATIENT TESTIMONIALS
Recent Awards
We are honored and deeply appreciative to have consistently received prestigious awards and recognition year after year, establishing us as one of New York’s foremost hospitals for a wide range of general surgeries, safety measures, specialized procedures, and overall excellence in healthcare. At Lenox Hill Minimally Invasive Surgery, our unwavering commitment lies in delivering exceptional care and unwavering support to our patients, guaranteeing their safety and successful recovery throughout their entire surgical experience.
Hospital Quality Awards
 America’s 50 Best Hospitals Award™ (2023, 2022)
America’s 50 Best Hospitals Award™ (2023, 2022)
Top 1% in the nation for providing the highest clinical quality year over year.

America’s 100 Best Hospitals Award™ (2021)
Top 2% in the nation for consistently delivering clinical quality year over year.

America’s 250 Best Hospitals Award™ (2023, 2022, 2021)
Top 5% in the nation for consistently delivering clinical quality.

Patient Safety Excellence Award™ (2023, 2022)
Top in the nation for providing excellence in patient safety by preventing infections, medical errors, and other preventable complications.
Specialty Clinical Quality Awards

America’s 100 Best Hospitals for Cardiac Care Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in heart bypass surgery, coronary interventional procedures, heart attack treatment, heart failure treatment, and heart valve surgery.

America’s 100 Best Hospitals for Coronary Intervention Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in coronary intervention procedures (angioplasty with stent).

America’s 100 Best Hospitals for Prostate Surgery Award™ (2023, 2022, 2021)
Superior clinical outcomes in prostate removal surgery and transurethral resection of the prostate.
Click to see all of our Healthgrades best doctors awards


Visit our main website at www.LenoxHillMinimallyInvasiveSurgery.com
Blog Posts are Below:
Category Archives: Pancreas Surgery
Pancreas Surgery: Management of Pancreatic Diseases through Surgery
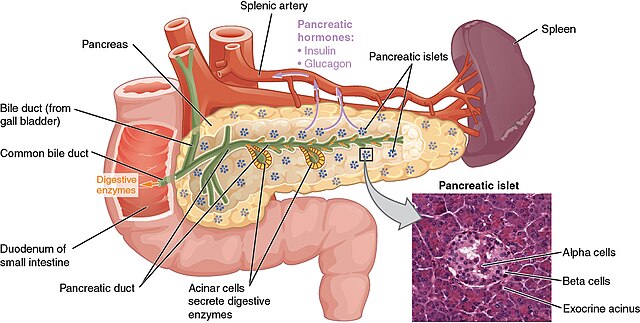
When is pancreas surgery necessary? The pancreas is a vital organ located behind the stomach, responsible for producing digestive enzymes and regulating blood sugar through hormone production. When pancreatic diseases occur, they can have severe consequences on overall health. For conditions that cannot be managed through medication or lifestyle changes, pancreas surgery often becomes a necessary treatment option.

In this comprehensive guide, we’ll explore common pancreatic diseases that may require surgery, the different types of pancreatic surgeries, the latest advancements in surgical techniques, and what patients can expect during recovery.
Common Pancreatic Diseases Requiring Surgery
Several conditions affecting the pancreas may necessitate surgical intervention. Here are some of the most common pancreatic diseases that often require surgical management:
1. Pancreatic Cancer
Pancreatic cancer is one of the most serious forms of cancer, often diagnosed at an advanced stage due to its subtle symptoms. The most common type is pancreatic ductal adenocarcinoma, which typically originates in the ducts of the pancreas. Surgery is a primary treatment for pancreatic cancer, especially if it’s localized and detected early.
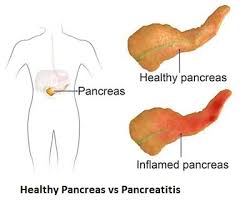
2. Pancreatitis
Pancreatitis is the inflammation of the pancreas, which can be acute or chronic. Acute pancreatitis is usually a sudden condition that may resolve with conservative treatment, while chronic pancreatitis is a long-term, progressive inflammation often due to repeated bouts of acute pancreatitis, gallstones, or alcohol use. Surgery may be recommended for chronic pancreatitis when there’s persistent pain, blockage, or other complications.
3. Pancreatic Cysts and Neoplasms
Pancreatic cysts and benign neoplasms are growths in the pancreas. While many pancreatic cysts are benign, some have the potential to become cancerous over time. Surgery may be required to remove cysts if they are symptomatic, large, or carry a risk of malignancy.
4. Neuroendocrine Tumors
Pancreatic neuroendocrine tumors (NETs) are a rare type of tumor that originates in the hormone-producing cells of the pancreas. These tumors can be either benign or malignant and may produce symptoms related to excess hormone production. Surgery is often the first line of treatment, especially if the tumor is localized and can be safely removed.
Types of Pancreatic Surgery
The type of surgery performed on the pancreas depends on the specific disease, its location, and the stage at which it is diagnosed. Here are some of the most common pancreatic surgical procedures:
1. Whipple Procedure (Pancreaticoduodenectomy)
The Whipple procedure, or pancreaticoduodenectomy, is the most common surgery for pancreatic cancer located in the head of the pancreas. During this complex procedure, the surgeon removes the head of the pancreas, part of the small intestine (duodenum), the gallbladder, and sometimes part of the stomach. The remaining organs are then reconnected to allow for normal digestion. Although it is a major surgery, the Whipple procedure is often the best option for treating cancers in the head of the pancreas.
2. Distal Pancreatectomy
In a distal pancreatectomy, the tail (and sometimes part of the body) of the pancreas is removed, leaving the head intact. This procedure is commonly performed for tumors or cysts located in the tail of the pancreas. In some cases, the spleen may also be removed if it is affected or if it will facilitate a safer procedure.
3. Total Pancreatectomy
A total pancreatectomy involves the removal of the entire pancreas. This procedure is usually reserved for cases where cancer or disease affects the entire pancreas and cannot be treated by removing only part of the organ. After a total pancreatectomy, the patient will require lifelong enzyme replacement and insulin therapy, as the body will no longer be able to produce insulin or digestive enzymes.
4. Enucleation
Enucleation is a less invasive procedure often used to remove small, benign pancreatic neuroendocrine tumors. During enucleation, only the tumor is removed, preserving as much of the healthy pancreas tissue as possible. This procedure is ideal for small, well-defined tumors that do not invade nearby structures.
Advances in Minimally Invasive Pancreatic Surgery
Recent advancements in surgical technology have made minimally invasive approaches more accessible and effective for pancreatic surgery. Minimally invasive techniques, including **laparoscopic** and **robotic-assisted surgery**, offer patients significant benefits compared to traditional open surgery.
- Laparoscopic Surgery: This minimally invasive approach uses small incisions and a laparoscope (a thin tube with a camera) to guide the surgery. Surgeons can perform complex pancreatic procedures with greater precision and minimal trauma to surrounding tissues.
- Robotic-Assisted Surgery: Robotic-assisted surgery enhances the surgeon’s dexterity and control, allowing for more precise movements in delicate areas. This approach is especially beneficial for complex procedures, as it reduces the likelihood of complications and often results in faster recovery times.
The benefits of minimally invasive pancreatic surgery include:
- Smaller incisions and less scarring
- Reduced post-operative pain
- Shorter hospital stays and faster recovery times
- Lower risk of infection and complications
Recovery After Pancreatic Surgery
Recovery from pancreatic surgery depends on the type of procedure performed and the patient’s overall health. Here’s what most patients can expect during recovery:
- Hospital Stay: Pancreatic surgeries are major procedures, often requiring a hospital stay ranging from a few days to two weeks, depending on the complexity of the surgery and any complications.
- Pain Management: Pain is common after pancreatic surgery, especially with open procedures. Pain management techniques include medications and, in some cases, epidural or nerve block anesthesia for the first few days.
- Dietary Adjustments: After surgery, patients will need to follow a special diet to allow the pancreas to heal. This usually starts with a liquid diet, followed by soft foods. Patients may also require enzyme supplements to aid in digestion, especially if a large part of the pancreas was removed.
- Lifelong Management: For patients who undergo a total pancreatectomy, lifelong enzyme replacement and insulin therapy are necessary. Even with partial removal, patients may need ongoing management to control blood sugar levels and support digestion.
Success Stories and Improvements in Quality of Life
Pancreatic surgery can be life-changing for patients dealing with chronic pain, cancer, or other debilitating symptoms due to pancreatic diseases. Success stories often highlight patients who have regained control of their health, with significantly improved quality of life. Some individuals with pancreatic cancer have been able to achieve remission through early intervention and surgery, while others suffering from chronic pancreatitis have been able to live pain-free after successful surgical treatment.
The improvements in minimally invasive techniques and post-operative care have increased the success rates of pancreatic surgeries, allowing patients to enjoy better outcomes and faster recovery times.
When to Consider Pancreas Surgery
Patients diagnosed with serious pancreatic conditions should consider surgery as a treatment option if recommended by their healthcare provider. Early intervention is key for the best outcomes, particularly in cases of pancreatic cancer or neuroendocrine tumors. Discussing the benefits, risks, and long-term impacts of surgery with a general surgeon specializing in pancreatic diseases can help you make an informed decision about your treatment plan.
If you or a loved one is facing a pancreatic disorder that may require surgery, consulting with a team of skilled surgeons can make all the difference in your recovery journey.
Contact Lenox Hill Minimally Invasive Surgery today to schedule a consultation and learn more about the latest advancements in pancreatic surgery and how our experienced team can help you on the path to restored health.
Contact Information
LENOX HILL MINIMALLY INVASIVE SURGERY
117 E 77th Street
New York, NY 10075
646-846-1136
admin@lenoxmis.com
Visit our website for more information: https://lenoxhillminimallyinvasivesurgery.com/
Pancreas Disease and Surgery
This article will cover important information about pancreas disease and surgery. The pancreas is a pivotal organ of the human body. It is responsible for the regulation of vital enzymes inside the body. These enzymes help regulate important chemical processes inside the body. Furthermore, it also produces insulin, which is an essential chemical that controls the blood sugar level. Enzymes and chemicals such as these help you absorb micro and macronutrients. Not to mention, the Pancreas plays an emphatic role in the digestion process as well.
Pancreatic Disorders
Pancreatic disorders are one of the toughest medical issues to treat. The two most serious pancreatic disorders are exocrine pancreatic insufficiency (EPI) and pancreatitis. EPI is an extremely harmful disorder that can lead to chronic pancreatitis.
Other disorders in the pancreas include cystic fibrosis, diabetes, and pancreatic cancer. Each of these conditions comes with varying symptoms and causes.
Pancreatitis
Condition of pancreatitis is the inflammation of the pancreas. An individual can have three types of pancreatitis, acute, chronic, and hereditary. Each of these three types constitutes a different cause and severity.
Acute Pancreatitis
Acute pancreatitis can be an underlying cause of another condition, such as gallstones. It is a short term and sudden inflammation that you can face due to excessive use of harmful substances. These substances include drugs, alcohol, and unhealthy edibles that influence hormonal imbalance in the body. Therefore, any abnormalities in the electrolytes and lipids can lead to acute pancreatitis.
The pain associated with this condition is very severe. You can expect intense pain in the upper abdomen region, followed by nausea, vomiting, diarrhea, and fever. Apart from the many habitual triggers of this disease, it can also be a result of inheritance. Hence, doctors carry out the treatment for this disease according to the cause.
Chronic Pancreatitis
Unlike acute pancreatitis, the development of chronic pancreatitis is slow and progressive. Therefore, the symptoms gradually occur and can last much longer than acute pancreatitis. This condition can also lead to exocrine pancreatic insufficiency. A person suffering from chronic pancreatitis encounters symptomatic episodes of diarrhea and abdominal discomfort.
One can also begin to lose weight. The slow progression of this disease can cause long-term damage to the pancreas. Lastly, since the pancreas regulates the blood glucose level and nutrient absorption, a person with chronic pancreatitis becomes highly vulnerable to diabetes and malnutrition.
Hereditary Pancreatitis
Like chronic pancreatitis, hereditary pancreatitis is also a progressive condition. Genetic mutations cause the occurrence of this condition in an individual. With this disease, a person can start showing symptoms as early as 30 years old. Further complications will also cause a person to develop the symptoms of chronic pancreatitis. Doctors usually treat this condition with the help of PERT and pain management.
EPI (Exocrine Pancreatic Insufficiency)
EPI is a condition that makes a person highly enzyme deficient. The deficiency of enzymes can lead to severe consequences. The pancreas loses its functionality to release nutrient-absorbing enzymes and causes malnourishment. Another indication of this disorder is the excessive fat in a person’s stool.
Surgery for Pancreatitis
A doctor resorts to surgical solutions for pancreatitis when the pancreas becomes unable to secrete essential fluids. This inability is usually due to tissue scarring of the pancreas, which the inflammation causes. Surgeons will either create a new passageway from the pancreas to the small intestine to exhibit the flow of the fluids. Alternatively, the surgeons will remove the infected tissue from the pancreas.
Lateral Pancreaticojejunostomy
This surgical procedure heals the central part and the tails of the pancreas. This particular surgical approach involves the surgeons operating on the pancreatic duct. This duct is an organic tube that covers the pancreas and makes the essential fluids flow inside.
The surgeons take this duct and attach it to the small intestine, where most of the digestion and absorption takes place. By doing so, the doctors counter the problems with nutrient absorption. Once they form the connection between the digestive enzymes and the food particles, the patient starts to build back their nutrition intake.
Pancreatic Resection
Surgeons decide to take this surgical approach when the infectious cavity starts causing massive damage to the pancreas. The spread of inflammation in a muscle cavity will cause the pancreas muscles to die. In this case, the doctor needs to proceed with a pancreatic resection to stop the inflammation from causing further destruction. For this procedure, the doctor removes the infectious areas of the pancreas to keep it from spreading and causing other complications.
Recovery
The recovery time of the surgery can depend on the type of the surgery also your condition. Open surgery usually accounts for a longer recovery time because the incision wound needs rest time to heal. However, if the surgeon uses another technique in which the incisions are small, then you can expect the recovery to be faster.
Pancreas Disease and Surgery: To Conclude
If you or anyone you know are suffering from pancreatic problems, then visit Lenox Hill Minimally Invasive Surgery. We provide you with the best surgeons, specialized in treating pancreas diseases. Visit our website or call us today to schedule an appointment:
LENOX HILL MINIMALLY INVASIVE SURGERY
117 E 77th Street
Suite 1A
New York, NY 10075
Phone: 646-846-1136
Email: admin@lenoxmis.com
Types of Pancreas surgery
The pancreas plays an important role in human digestion. One of its major functions is to release the hormones insulin and glucagon that regulate the blood sugar level. The diseases and disorders of pancreas like pancreatitis are less common, and the treatment requires no surgery. However, a surgery is inevitable when treating a severe disorder or removing a tumor.
Types of Pancreas surgery
Open surgery and laparoscopy are the options available for the pancreas surgery. Open surgery involves either the removal of a certain part of the pancreas where the tumor is growing or the removal of other parts of digestive organs as well like gall bladder, stomach, small intestine, and common bile duct. The type of surgery depends upon the stage of cancer.
Whipple Procedure:
Whipple procedure or pancreatic resection involves the removal of the pancreatic head, duodenum of the small intestine, gall bladder and bile duct. This surgical procedure treats pancreatic cancer and other disorders of the pancreas. Whipple procedure is a complex and risky surgical treatment, but very effective and life-saving for treating pancreatic cancer, pancreatitis, bile duct cancer, serious trauma or injury in the pancreas and ampullary cancer.
Distal Pancreatectomy:
The name of the procedure that involves the removal the left side of the pancreas ( body and tail) to eradicate the growing tumor is distal pancreatectomy. Your surgeon might need to remove the spleen attached with pancreas as well.
Total Pancreatectomy:
Total pancreatectomy is the removal of the pancreas when tumor has spread all over the pancreas. Other common procedures cannot treat this issue. You can live without pancreas normally. However, you will need a supply of insulin, glucagon, and other important hormones and enzymes.
Laparoscopy Surgery for the Pancreas:
Minimal Invasive Laparoscopy for pancreas involves removing the tumor or a small part of the pancreas with small incisions. Your surgeon will make three to four keyhole incisions in your pancreas and remove the infected or injured portion with tumor growth.
Pseudocyst Drainage:
The pancreatic disorder includes the production of cysts in the pancreas. Cysts in the pancreas are large fluid-filled sacks that can disturb the normal functioning of the pancreas and can even turn cancerous. Pseudocyst drainage involves inserting a tube or needle into the cysts or pseudocysts to drain the cysts from the pancreas.
Islet Cell Transplant:
Islet cells in the pancreas are responsible for the production of insulin. Impairment in islet cells leads to an insufficient production of insulin leading to Diabetes type 1. Islet cell transplantation can potentially cure diabetes. Healthy islet cells from the donor are harvested and transplanted into the pancreas of the patient.
Risks of Pancreatic Surgery:
To have the best outcome of the pancreas surgery, it is crucial to have the surgery from a highly qualified and experienced surgeon. In rare cases, there can be come complications. The complications include bleeding, infection, development of diabetes ( temporary or permanent), leaking, etc. if the surgeon fails to join the organs after removing multiple parts from the digestive system. The pancreas surgery can lead to weight loss and change in the bowel functions.
Lenox Hill Minimally Invasive Surgery have NYC’s best and most qualified surgeons for treating pancreatic cancers and disorders. With Lenox Hill Minimally Invasive Surgery your pancreatic surgeries are complication-free. We promise to provide you the best treatment for your surgery and quick recovery.
Call us at 212-988-1136
Visit lenoxhillminimallyinvasivesurgery.com to learn more.
Pancreas Surgery – What to Expect
Pancreaticoduodenectomy – what a mouthful! This long word is the technical name for one of the most common pancreas surgery procedures. Also known as the Whipple procedure, this surgery involves removing a diseased section of the pancreas. But what even is the pancreas? Why do we need it? And what should you expect if you need this surgery?
What is the Pancreas?
Many people would likely have difficulty pointing up the location of the pancreas, let alone naming what it does. The pancreas can be found in the abdomen, just behind the stomach. It is a small organ, not more than a few inches long, but one of the most essential organs for daily life. The pancreas is responsible for the creation of specific chemicals that the body uses for digestion. These chemicals, also known as enzymes, are used to break down the food that we eat. without these enzymes, we would be unable to process the fat, proteins, and carbs within our food into energy.
At the same time, the pancreas also responsible for creating the two hormones that monitor and regulate blood sugar- insulin and glucagon. In cases where the pancreas is unable to produce the hormones and enzymes it should, serious and life-threatening side effects can develop.
Why Would you Need Pancreas Surgery?
When functioning properly, the pancreas is an essential organ for regulating energy levels and providing the body with the nutrients it requires. However, in some cases, the pancreas can pose a potential threat to the rest of the body. For example, in the case of pancreatitis, those enzymes used to digest food begin the process of digestion on the pancreas itself.
Other times, the pancreas can develop cancer. This can be a serious risk, as cancer can spread to other parts of the body. This makes the pancreas a risk to the other organs within the body.
What to Expect from Pancreas Surgery
During the procedure for pancreas surgery, you will be anaesthetized and the surgeons will do what they do best. Depending on your specific needs, they may remove certain sections of the pancreas and even surrounding tissue. Usually, the general needs can be identified long before the surgery starts. Some decisions need to be made while the surgery is happening. That is why you want to have the best surgeons you can find working with you!
Once the surgery has been completed, a short stay is to be expected. This gives us an excellent opportunity to closely monitor your recovery, vital signs, and medication use to ensure you are healing properly. Your stay will likely not be more than a few days, but full recovery from pancreas surgery can take up to a few months. While you recover, there are a few side effects and changes you can expect. The first and most common is operation site pain or discomfort. Digestive problems have also been noted. As the pancreas plays such a large part in digestion, it is only to be expected that the body will have to adjust to a new way of doing things. The most noteworthy aspect of this is the fact that you will not be able to eat for a few days after the surgery.
Any time there is a procedure near the abdomen, there is a potential for essential skills such as walking and sitting up to be impaired. It will be important to, in accordance with your specific instructions from your surgeon, stay active to the extent possible.
Are you in need of pancreas surgery? Call the best surgeons in NYC for a consultation today.
LENOX HILL MINIMALLY INVASIVE SURGERY
——————-
References
https://www.pancreaticcancer.org.uk/information-and-support/treatments-for-pancreatic-cancer/surgery-for-operable-pancreatic-cancer/types-of-surgery/
https://www.cancer.org/cancer/pancreatic-cancer/treating/surgery.html
http://columbiasurgery.org/pancreas/what-expect-after-operation
Pancreas Surgery – NYC General Surgeon
Pancreas Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
 The pancreas being a key organ of the endocrine and digestive systems of the body is indispensable for the smooth functioning of the human body. Hence, a diseased condition of the pancreas, like a tumor, abscess or malignancy that causes pancreatitis and makes the dysfunctional organ calls for pancreatic surgery. There are different methods, or kinds of pancreas surgery and the type that a patient will have to opt for will depend upon whether his or her pancreatitis is chronic or acute.
The pancreas being a key organ of the endocrine and digestive systems of the body is indispensable for the smooth functioning of the human body. Hence, a diseased condition of the pancreas, like a tumor, abscess or malignancy that causes pancreatitis and makes the dysfunctional organ calls for pancreatic surgery. There are different methods, or kinds of pancreas surgery and the type that a patient will have to opt for will depend upon whether his or her pancreatitis is chronic or acute.
More often than not, the condition or syndrome can be treated and managed without going for invasive intervention or surgery. Nevertheless, if an infection or degeneration of the pancreatic tissues becomes longstanding and acute, surgery is the only treatment option.
Steps
 The most common pancreatic surgery procedures include minimally invasive pancreatic resection, spleen-preserving pancreatectomy, ‘The Whipple’, and Enucleation of pancreatic tumor.’ Minimally invasive pancreatic resection surgery is conducted laparoscopically giving the interventional radiologist or gastroenterologist good access to the abdomen via tiny keyhole notches. This surgical method is appropriate for patients having pancreatic cysts.
The most common pancreatic surgery procedures include minimally invasive pancreatic resection, spleen-preserving pancreatectomy, ‘The Whipple’, and Enucleation of pancreatic tumor.’ Minimally invasive pancreatic resection surgery is conducted laparoscopically giving the interventional radiologist or gastroenterologist good access to the abdomen via tiny keyhole notches. This surgical method is appropriate for patients having pancreatic cysts.
Spleen-preserving pancreatectomy is conducted laparoscopically where the pancreas is excised, but the spleen is kept intact for preserving its immunological functionality as well as minimize the risks of complications and infections in the future. The traditional pancreatectomy method entails the removal of the spleen along with the metastatic pancreas for reversing the spread of cancer. Nevertheless, if the surgery is carried out for a benign condition like pancreatic tumor or cyst, then spleen resection is not necessary.
Enucleation process is appropriate for dealing with benign or non-cancerous tumors where these are scraped out carefully instead of expurgating a large pancreatic section.
‘The Whipple’ surgery or ‘pancreaticoduodenectomy’ is the go-to procedure for treating pancreatic cancer and also for dealing with complications or abscesses related to the bile duct, intestine, and pancreas. The surgery where the top of the pancreas, bile duct, gallbladder, and duodenum are removed can be extremely complex and demanding, fraught with risks.
Benefits
If the surgery is for treating pancreatitis or tumors, then opting for laparoscopic surgery is the best option. In such a case, recuperation is faster necessitating a shorter hospital stay. However, if the surgery is for pancreatic cancer, then the operation lasts for several hours and the patient may have to be in the hospice for at least a week.
Complete recovery might take many weeks and even months. Benefits of going for a major pancreatic surgery are:-
- Best treatment technique for remedying cancer and reversing chronic pancreatitis
- Increased lifespan
- Digestive issues and complications associated with pancreas might be resolved post surgery
- Chemotherapy and radiotherapy for continued treatment in case cancer recurs
Side Effects
Pancreatic surgeries for dealing with cancer tend to be extremely complicated, and it is no wonder that such operations have a very high mortality rate. Nearly 50% of the patients report grave complications and about 2%-4% expire. The most common risks include:-
- Wound infection or cardiac infection
- Hemorrhage (bleeding)
- Leakage from pancreas from the point where it is linked with the intestine
- Allergic reaction to general anesthesia (very rare)
Precautions
Fully recuperating from a complex pancreas surgery takes time and the convalescing process could be exhausting, especially for older patients. You’ll be required to report to your surgeon 1-2 times in a month following your recovery. The doctor will evaluate your progress and may recommend CT or MRI scans, and blood tests to ensure that there is no recurrence of cancerous tumors or lesions.
Dietary and lifestyle changes to have to be made to maintain overall health and also to reduce the risks of relapse.
Prognosis
Pancreatic cancer and all other serious complications of the pancreas are, by and large, regarded as untreatable and hence incurable. Nevertheless, the mortality rates related to pancreatic cancer (post surgery) have steadily declined over the decades.
Concluding Remarks
Living without a pancreas can be a challenge for any individual. If you’re diagnosed with a tumor or inflammation of your pancreas, you can continue to live an almost normal life, provided you opt for an appropriate treatment plan and abide by our physician’s guidelines. If you’ve cancer, then surgical removal of the pancreas is the only option. However, you’ll have to keep your fingers crossed on whether cancer will recur or not.
References
- https://www.mayoclinic.org/tests-procedures/whipple-procedure/about/pac-20385054
- https://stanfordhealthcare.org/medical-treatments/c/cancer-surgery/types/complex-pancreatic-surgery.html
- https://www.mskcc.org/blog/drug-reduces-risk-serious-pancreatic-surgery-complication
- https://stanfordhealthcare.org/medical-treatments/p/pancreatic-surgery/types/spleen-preserving-pancreatectomy.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2023932/
- https://www.ariahealth.org/programs-and-services/surgery/general-surgery/pancreatic-surgery
- http://columbiasurgery.org/pancreas/what-expect-after-operation
- https://www.cancer.org/cancer/pancreatic-cancer/treating/surgery.html
- http://pancreatic.org/pancreatic-cancer/about-the-pancreas/prognosis/