CALL TODAY 646-846-1136 | EMAIL
Surgical Experts Dedicated to Improving Lives
At Lenox Hill Minimally Invasive Surgery PLLC, Dr. Valery Dronsky and his staff of medical professionals provide compassionate care with the highest ethical & professional standards. In our state of the art facility, we offer surgical services using only the most cutting edge and current procedures and treatments. We specialize in general surgery, including extensive experience in performing hernia repair surgery. Our expertise is in minimally invasive surgery and robotic surgery. Minimally invasive and robotic surgery often allow patients to experience easier recovery than traditional open surgery. They also allow for more precise and less traumatic surgery. When robotic and minimally invasive surgery is not an option, we are also skilled and experienced in traditional open surgical procedures.
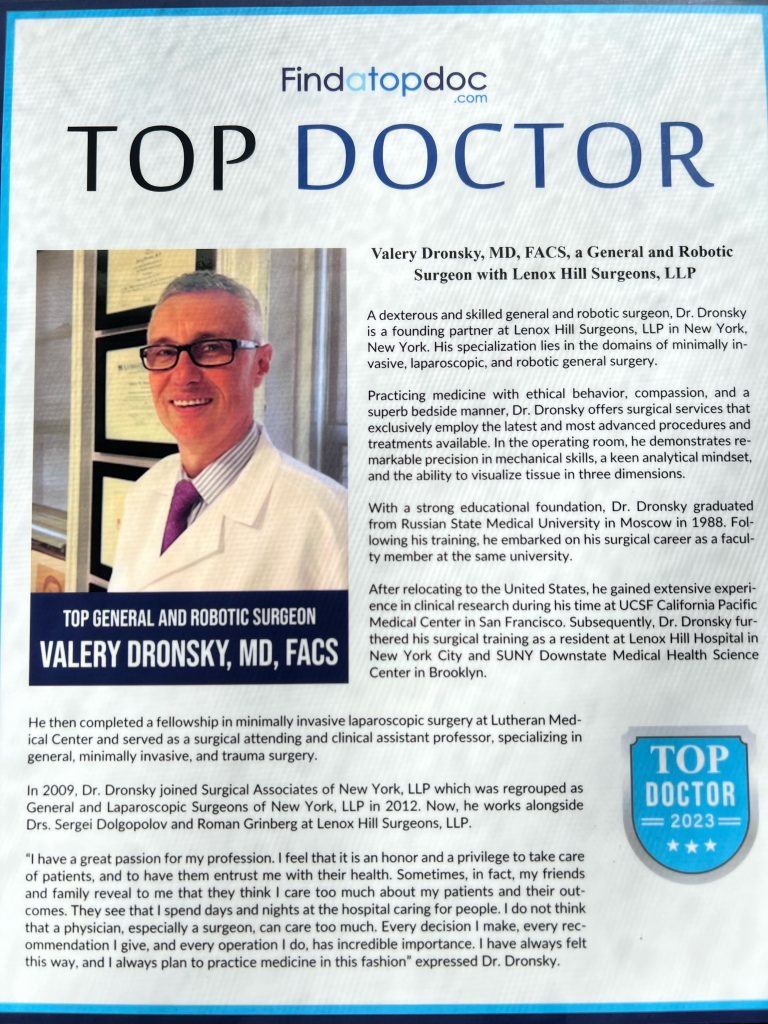
Dr. Dronsky is an experienced and highly skilled surgeon having undergone extensive training in school, residency and fellowships. He practices medicine with ethical behavior, compassion and superb bedside manner. In the operating room he exhibits precision mechanical abilities, analytical thinking and the ability to visualize tissue in three dimensions. These innate and learned skills allow Dr. Dronsky to be one of the most dexterous and skilled professionals in New York City and the Country.
Call us: 646-846-1136
PATIENT TESTIMONIALS
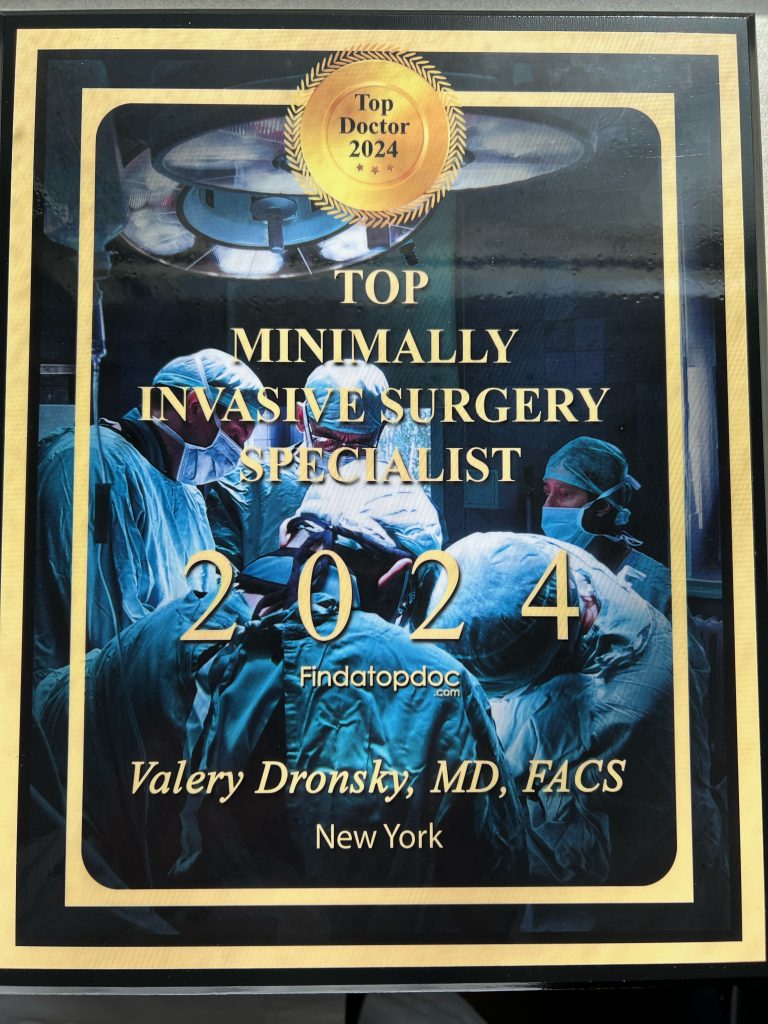
Recent Awards
We are honored and deeply appreciative to have consistently received prestigious awards and recognition year after year, establishing us as one of New York’s foremost hospitals for a wide range of general surgeries, safety measures, specialized procedures, and overall excellence in healthcare. At Lenox Hill Minimally Invasive Surgery, our unwavering commitment lies in delivering exceptional care and unwavering support to our patients, guaranteeing their safety and successful recovery throughout their entire surgical experience.
Hospital Quality Awards
 America’s 50 Best Hospitals Award™ (2023, 2022)
America’s 50 Best Hospitals Award™ (2023, 2022)
Top 1% in the nation for providing the highest clinical quality year over year.

America’s 100 Best Hospitals Award™ (2021)
Top 2% in the nation for consistently delivering clinical quality year over year.

America’s 250 Best Hospitals Award™ (2023, 2022, 2021)
Top 5% in the nation for consistently delivering clinical quality.

Patient Safety Excellence Award™ (2023, 2022)
Top in the nation for providing excellence in patient safety by preventing infections, medical errors, and other preventable complications.
Specialty Clinical Quality Awards

America’s 100 Best Hospitals for Cardiac Care Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in heart bypass surgery, coronary interventional procedures, heart attack treatment, heart failure treatment, and heart valve surgery.

America’s 100 Best Hospitals for Coronary Intervention Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in coronary intervention procedures (angioplasty with stent).

America’s 100 Best Hospitals for Prostate Surgery Award™ (2023, 2022, 2021)
Superior clinical outcomes in prostate removal surgery and transurethral resection of the prostate.
Click to see all of our Healthgrades best doctors awards


Visit our main website at www.LenoxHillMinimallyInvasiveSurgery.com
Blog Posts are Below:
Category Archives: best general surgeons nyc
General Surgery: Colon Cancer
People with colon cancer mostly have to undergo general surgery. It is the primary treatment for people with early stages of colon cancer. Furthermore, there are different types of colon surgeries. The doctors choose to perform between each of the surgery by considering certain factors. These factors involve the severity of cancer, location of the abnormal growth in the colon, and the exact purpose of the surgery.
Polypectomy
Surgeons use this type of colon surgery procedure for patients that are just in the early stages of tumor. In this stage, polyps start to spear in the colon. These polyps are small abnormal growth in the colon that share the size of a mushroom. In hindsight, they look like small bumps or dents in the colon.
Since polyps do not cause sizable disruption, a doctor can simply use a colonoscopy tube to get rid of them. A polypectomy is a procedure in which the doctor inserts a long tube inside a patient and attaches a camera to it. The camera helps the doctor navigate around the colon to look for cancerous polyps.
After the careful spotting of the polyp, the doctor uses a wire to loop around the stem of the polyp and then cut it off with the help of an electric current. This a very careful procedure; the doctor takes plenty of precautions before they can remove the cancerous cavity. Nevertheless, it is relatively easier and less time consuming than other surgeries for colon cancer.
Local Excision
Local excision is another minimally invasive procedure like polypectomy. For procedures such as these, the doctor does not have to make incisions in the stomach. However, this procedure requires slightly more involvement from the professional. The doctor not only removes the cancerous polyps inside the colon but also the surrounding healthy tissues.
This prevents further spread. However, this does not promise the prevention of further growth of cancerous cells. If the doctor believes that the cancer is likely to spread, then they will opt for another procedure, such as Colectomy.
Colectomy
Colectomy is one of the solutions to treat colon cancer. The doctor removes the colon or some parts of the colon in this surgery. The doctor decides whether they will perform a total colectomy or partial colectomy depending on the intensity of the abnormal growth.
Partial Colectomy
In a partial colectomy, surgeons remove one-third or one-fourth of the colon along with some of the lymph nodes so they can check them for cancer. This surgery only removes the portion of the colon that has cancerous growth and then sews the remaining colon together. You can also call this surgery segmental colectomy and hemicolectomy.
Total Colectomy
In a total colectomy, a person undergoes a complete colon removal. The doctor goes for this option when the polyp growth extends beyond control. Furthermore, doctors may also resort to this solution when the person with colon cancer starts having other problems with their colon.
Colostomy
If the doctor is unable to instantly sew the colon together after partial colectomy, then the patient undergoes a colostomy. For this surgery, the doctor attaches a colostomy bag to the colon until the other part of the colon heals. The plastic bag allows the patient to pass stool from the colon since the bag acts as a collective source of the stool. The bag directly attaches to the stoma of the colon; the stoma is the opening of the operated colon.
Colectomy – The Procedure
There are two ways a doctor can perform a colectomy: Open colectomy and laparoscopic-assisted colectomy.
Open Colectomy
For this procedure, the doctor makes a long incision in the abdominal region of the body. Surgeons use a scalpel for this surgery, and it creates an opening into the colon for operation.
Laparoscopic Assisted Colectomy
Unlike open surgery, the surgeons make multiple small incisions and use a laparoscope, along with other tools to perform this operation. The laparoscope is a long and thin tube, having a micro camera and lights at the end of it. This allows surgeons to move around the abdomen with the help of this tool and have clear visibility. In comparison to open colectomy, this procedure is less invasive.
Since the incisions in this procedure are small, the patient recovery time decreases to a significant amount. Thus, a patient does not have to be under bed rest for too long in this surgery. Nevertheless, this is a much more technical procedure because of the use of highly advanced tools. Only surgeons that have the expertise and experience of performing a laparoscopic surgery will offer you the best procedure.
General Surgery Colon Cancer: Consult with Experienced Surgeons
If you want access to professional and expert colon surgery in New York, then head on to Lenox Hill Minimally Invasive Surgery. We offer the best surgical services, along with the expertise of surgeons that specialize in colon surgery. Visit our website now, or call us at 646-846-1136 to book an appointment.
NYC General Surgeons Discuss Rheumatoid Arthritis
What is Rheumatoid Arthritis?

According to the Arthritis Foundation, there are approximately 1.5 million Americans who are living with rheumatoid arthritis right now. Both men and women can develop it, but statistics show that women are almost three times more likely to suffer from the condition. If you have recently been diagnosed with rheumatoid arthritis, or suspect you may have it, it’s imperative to learn all you can so you can find the best treatment plan for your specific needs.
Understanding Rheumatoid Arthritis

Classed as a chronic inflammatory autoimmune disorder, rheumatoid arthritis can severely affect a number of areas on a person’s body. While many people assume it just affects the joints, it doesn’t stop there. Rheumatoid arthritis can also affect a person’s heart, lungs, blood vessels, eyes, and even their skin. When a person has rheumatoid arthritis, their own body turns against itself and starts attacking the tissue.
Over time, it can cause swelling which is exceptionally painful, joint deformity, and even bone erosion.
What Are the Signs and Symptoms?

In the beginning stages of rheumatoid arthritis, typically the person may notice stiffness of the joints after activity or, in the morning, swollen joints, tender joints – joints that feel warm to the touch. Weight loss, fatigue, and even a fever are other common symptoms.
While each case is different, it tends to start in the fingers and toes; in other words, the smaller joints.
What Are the Causes?
While doctors understand how rheumatoid arthritis develops, what they are unclear about is what actually sets off that motion or process. When a body’s immune system starts to attack the synovium, then the process begins.
Some doctors believe that genes play a big factor in determining whether or not you will develop it, while others point towards environmental factors and even certain bacterial viruses.
What Are the Treatment Options?
 Because rheumatoid arthritis gets worse over time, leaving it is not an option. You want to get a proper diagnosis as early as possible, and then start up with an appropriate course of action. Treatment can include a medication such as NSAIDs and/or steroids, as well as physical therapy.
Because rheumatoid arthritis gets worse over time, leaving it is not an option. You want to get a proper diagnosis as early as possible, and then start up with an appropriate course of action. Treatment can include a medication such as NSAIDs and/or steroids, as well as physical therapy.
In severe or advanced cases, it may be necessary to have a surgeon repair or even rebuild the tissue that has been damaged. This will help to prevent more problems down the road.
Contact us today to schedule an appointment with the best surgeons in Manhattan.
Top General Surgeons in Manhattan – Carpal Tunnel Surgery
What is Carpal Tunnel Syndrome?

Have you been feeling numbness, tingling, or even itching sensation in your fingers or hand as of late? Does it feel like you don’t have the same strength in your fingers and hand as you used to? If so, you may be suffering from carpal tunnel syndrome. This particular condition affects women more often than men, but that’s not to say that men aren’t at risk.
Here’s a closer look at the condition including what it is, who is at risk, what the signs and symptoms are, and what you can do about treatment:
Understanding Carpal Tunnel Syndrome Better
 Carpal tunnel syndrome occurs when there is added pressure being placed on your median nerve. This nerve is found in your arm and actually runs all the way down your arm, right into your wrist. The area in which the nerve runs into is called the carpal tunnel, thereby giving this condition its name.
Carpal tunnel syndrome occurs when there is added pressure being placed on your median nerve. This nerve is found in your arm and actually runs all the way down your arm, right into your wrist. The area in which the nerve runs into is called the carpal tunnel, thereby giving this condition its name.
The median nerve is an important one in that it helps to control feeling in your thumb and movement in your first three fingers. When you have carpal tunnel syndrome, there is swelling in that passageway, which then restricts motion and can cause pain.
Unfortunately, it doesn’t go away on its own, and it will only continue to get worse over time if no treatment is taken.
What Are the Signs and Symptoms?
The typical signs and symptoms include numbness, itching, tingling, and burning in your thumb, fingers, or even the palm of your hand.
Who Is At Risk of Developing It?
As for who is most at risk of developing carpal tunnel syndrome, that would be people who engage in repetitive motions. It’s not uncommon for it to be related to work, such as a person who spends much of their workday typing or using machinery.
But those aren’t the only people at risk. Those who are pregnant, have rheumatoid arthritis, are obese, have diabetes, or who have hypothyroidism are also at high risk.

What Are the Treatments Available?
The treatment plan will depend on the individual and the severity of the condition. The first step is usually lifestyle changes, and from there medication may be prescribed. If this fails, then surgery can end up being necessary. Surgery may be needed to reconstruct and even repair tissue that has been damaged.
For more information, contact us today at 646-846-1136 to schedule an appointment with the best plastic surgeon in Manhattan.
A Quick Guide to Appendix Surgery
 Appendix surgery NYC is one of the most common forms of surgery; it is also one of the safest. The appendix sits where the large and small intestines meet. It is a thin tube which is roughly four inches in length and in most people, it sits in the lower right abdomen.
Appendix surgery NYC is one of the most common forms of surgery; it is also one of the safest. The appendix sits where the large and small intestines meet. It is a thin tube which is roughly four inches in length and in most people, it sits in the lower right abdomen.
We still don’t know for sure what the function of the appendix is, but we have several theories. One theory is that the role of the appendix is to hold bacteria, to essentially ‘reboot’ the digestive system following a bout of diarrhea. Others believe that the appendix is an evolutionary hangover from our past when our diet was vastly different to today. It may have held digestive enzymes, which we no longer need as we have mastered the art of cooking food.
Conditions of The Appendix
The most common problem with the appendix is appendicitis. For reasons that we do not fully understand, the appendix can become inflamed and ultimately rupture. The most obvious symptom of this is an intense pain in the lower abdomen, often accompanied by nausea and vomiting.
Tumours of the appendix are rare but, fortunately, because a patient can easily survive without an appendix and without any impact on their quality of life, the prognosis is generally good so long as the cancer hasn’t metastasized. Carcinoid tumors periodically chemicals, which cause flushing, wheezing, and diarrhea. The other type of tumors found in the appendix is epithelial tumors, which are growths on the appendix that do not secrete chemicals.
Appendectomy
 Surgery to remove the appendix is known as an appendectomy and remains the only treatment for appendicitis that we know of. Traditionally, this surgery was performed by making a large incision in the patient’s abdomen to gain access to the appendix, but by using modern laparoscopic techniques, the surgeon only needs to make a small incision through which instruments can be used to cut the appendix into smaller pieces for removal. Surgery is also required to remove any tumors.
Surgery to remove the appendix is known as an appendectomy and remains the only treatment for appendicitis that we know of. Traditionally, this surgery was performed by making a large incision in the patient’s abdomen to gain access to the appendix, but by using modern laparoscopic techniques, the surgeon only needs to make a small incision through which instruments can be used to cut the appendix into smaller pieces for removal. Surgery is also required to remove any tumors.
Other Treatments
 While awaiting confirmation of a diagnosis, many doctors prescribe antibiotics to patients with a potential appendicitis, just in case the symptoms are being caused by an infection. It is also possible, albeit rather rare, for antibiotics to alleviate appendicitis. There is some evidence that in such cases patients are at a significant risk of relapse.
While awaiting confirmation of a diagnosis, many doctors prescribe antibiotics to patients with a potential appendicitis, just in case the symptoms are being caused by an infection. It is also possible, albeit rather rare, for antibiotics to alleviate appendicitis. There is some evidence that in such cases patients are at a significant risk of relapse.
Our clinic, with its team of dedicated and talented surgeons, offers the best appendix surgery NYC, so contact us for a consultation.
Contact us at 646-846-1136 to schedule an appointment.
The Benefits of Minimally Invasive Surgery
Surgery has certainly come a long way since the advent of modern medicine. While we have been able to perform surgeries for much of history, it is only relatively recently that we have been able to do so in anything resembling a safe environment. Now that we have a much better understanding of germs and safety standards and the importance of sterilized equipment, we can perform surgeries with ease. And with a good degree of confidence, we can also predict the outcomes. Generally, the patient outlook is very good and every year we are globally improving our knowledge and techniques.
One of the major technological innovations that have allowed us to perform surgeries that were previously impossible are the robots we now possess. These robots are capable of not only performing surgeries but doing so with a level of precision that is entirely impossible for a human to replicate.
Smaller Incisions
Even without robots, we can still perform keyhole surgeries, which allow surgeons to use precise tools to perform some types of surgery with only a very small opening in the skin. When only a minimal incision needs to be made then we can make the smallest possible cuts in skin and muscle.
Less Pain
Smaller and more precise wounds mean much less pain and this has several knock-on benefits for the patient. Higher pain levels are often associated with lower moods during recovery. America is also currently in the grip of an opioid epidemic and as a nation, we need to do more to wean ourselves of these addictive drugs. Powerful opioids do have legitimate uses, but their routine prescription is becoming problematic. Increased pain levels also have an effect on our stress levels, with higher levels of pain sometimes making sleeping, and occasionally eating, much more difficult. A lack of sleep and a poor diet are both contributing factors for depression, with the individual generally more susceptible to infections and illness.
Shorter Hospital Stay
The net effect of all the benefits of minimally invasive surgery NYC is that patients can recuperate much faster and so require less time in the hospital, freeing up beds for more patients.
Less Scarring
Smaller wounds mean less scarring, and with surgical scars being a significant contributor to body image issues after major surgeries, this is far more important than many people realize.
To find out more about minimally invasive surgery NYC, drop into one of our clinics for a consultation.
Contact us at 646-846-1136 to schedule an appointment.
General Surgery
Here are some brief descriptions about the different types of general surgery we perform:
Laparoscopic surgery
This is a relatively new specialty dealing with minimal access techniques using cameras and small instruments inserted through 0.3 to 1 cm incisions. Robotic surgery is now evolving from this concept (see below). Gallbladders, appendices, and colons can all be removed with this technique. Hernias are now repaired mostly laparoscopically. Most bariatric surgery is performed laparoscopically.[citation needed] General surgeons that are trained today are expected to be proficient in laparoscopic procedures.
Colorectal surgery
General surgeons treat a wide variety of major and minor colon and rectal diseases including inflammatory bowel diseases (such as ulcerative colitis or Crohn’s disease), diverticulitis, colon and rectal cancer, gastrointestinal bleeding and hemorrhoids.
Endocrine surgery
General surgeons are trained to remove all or part of the thyroid and parathyroid glands in the neck and the adrenal glands just above each kidney in the abdomen. In many communities, they are the only surgeon trained to do this. In communities that have a number of subspecialists, other subspecialty surgeons may assume responsibility for these procedures.
Surgical oncology
Surgical oncologist refers to a general surgical oncologist (a specialty of a general surgeon), but thoracic surgical oncologists, gynecologist and so forth can all be considered surgeons who specialize in treating cancer patients. The importance of training surgeons who sub-specialize in cancer surgery lies in evidence, supported by a number of clinical trials, that outcomes in surgical cancer care are positively associated to surgeon volume—i.e., the more cancer cases a surgeon treats, the more proficient he or she becomes, and his or her patients experience improved survival rates as a result. This is another controversial point, but it is generally accepted—even as common sense—that a surgeon who performs a given operation more often, will achieve superior results when compared with a surgeon who rarely performs the same procedure. This is particularly true of complex cancer resections such as pancreaticoduodenectomy for pancreatic cancer, and gastrectomy with extended (D2) lymphadenectomy for gastric cancer. Surgical oncology is generally a 2 year fellowship following completion of a general surgery residency (5-7 years).
Contact us at 646-846-1136 to schedule an appointment.
Recovering from a Lumpectomy
Recovering from a lumpectomy is, fortunately, typically a short process, but many women feel uneasy and are concerned about long-term effects, including the cosmetic effects of the surgery. Below is a quick guide to what to expect after a lumpectomy.
What Is a Lumpectomy?
A mass excision or lumpectomy is the removal of tissue believed to be cancerous from the breast. These lumps cannot necessarily be felt during an examination, but sometimes can show up during imaging scans. When suspect lumps are found, further diagnostics are performed by a radiologist, who will perform a wire localization with the aid of a mammogram or ultrasound. This will tell the surgeon where the lump is and allow for a more precise and smaller incision to be made.
How Is It Performed?
After making a small incision in the breast the surgeon then removes the lump and some of the surrounding tissue, although the surgeon will try to minimize surrounding tissue loss. Once the tissue has been removed, it will be handed to a pathologist who will analyze it to determine if it is cancerous or not and to ensure that there is no cancer in the outer layers of the surrounding tissue. If cancer is present here it would indicate that it has spread further from the source.
Sometimes the surgeon will also remove some tissue from the lymph nodes in the armpit to check that the cancer hasn’t spread to them. Also, the surgeon may insert some small metal clips into the area where tissue was removed, so that it shows up clearly on future imaging tests.
After the Procedure
Fortunately, recovery from a lumpectomy doesn’t take long and most women will not experience any serious pain or discomfort after the procedure.
The affected skin should heal in four weeks or so. Your doctor can advise you on how to look after the skin around the incision to promote healing. They will also explain to you how to change any dressings if necessary.
Most women can resume their usual routines and physical activities within a week but should avoid heavy lifting, jogging, and any activity which causes pain to the area, until two weeks after the procedure.
Prognosis
The prognosis following a lumpectomy depends on the size of the tumor and what the lab results say. If your lymph nodes are found to contain cancerous cells then there is a good chance of the cancer spreading.
Mass excision surgeries, such as lumpectomies, can seem scary. If you are facing a mass excision surgery of your own and have concerns then drop into our mass excision clinic for a consultation.