CALL TODAY 646-846-1136 | EMAIL
Surgical Experts Dedicated to Improving Lives
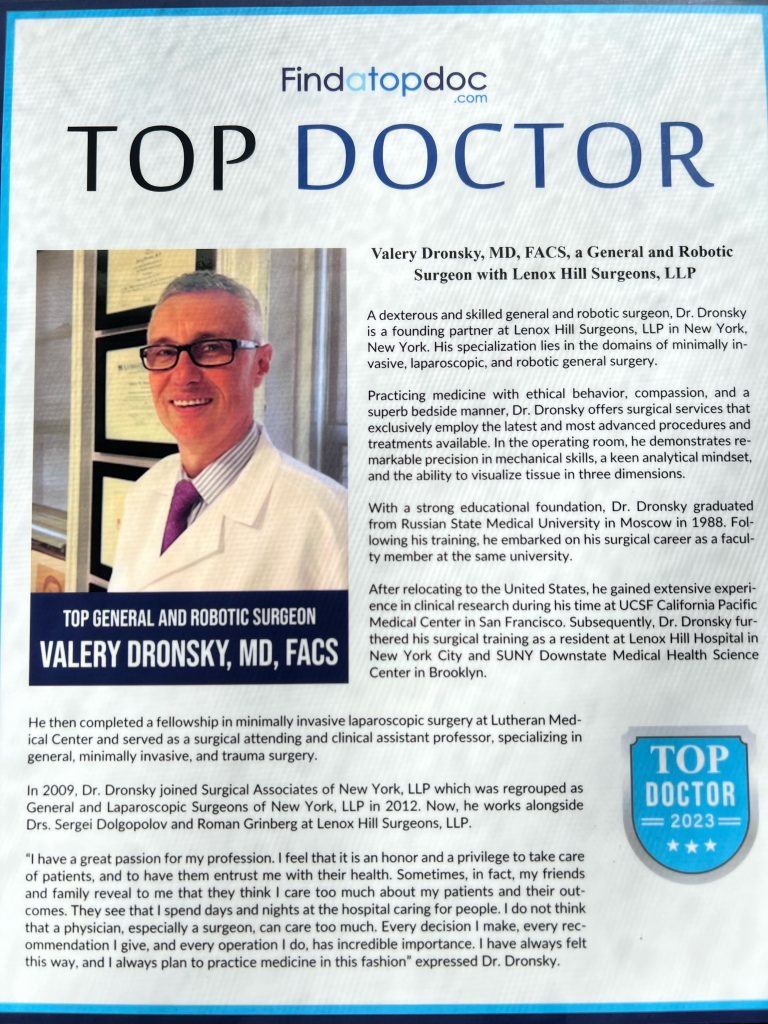
At Lenox Hill Minimally Invasive Surgery PLLC, Dr. Valery Dronsky and his staff of medical professionals provide compassionate care with the highest ethical & professional standards. In our state of the art facility, we offer surgical services using only the most cutting edge and current procedures and treatments. We specialize in general surgery, including extensive experience in performing hernia repair surgery. Our expertise is in minimally invasive surgery and robotic surgery. Minimally invasive and robotic surgery often allow patients to experience easier recovery than traditional open surgery. They also allow for more precise and less traumatic surgery. When robotic and minimally invasive surgery is not an option, we are also skilled and experienced in traditional open surgical procedures.
Dr. Dronsky is an experienced and highly skilled surgeon having undergone extensive training in school, residency and fellowships. He practices medicine with ethical behavior, compassion and superb bedside manner. In the operating room he exhibits precision mechanical abilities, analytical thinking and the ability to visualize tissue in three dimensions. These innate and learned skills allow Dr. Dronsky to be one of the most dexterous and skilled professionals in New York City and the Country.
Call us: 646-846-1136
PATIENT TESTIMONIALS
Recent Awards
We are honored and deeply appreciative to have consistently received prestigious awards and recognition year after year, establishing us as one of New York’s foremost hospitals for a wide range of general surgeries, safety measures, specialized procedures, and overall excellence in healthcare. At Lenox Hill Minimally Invasive Surgery, our unwavering commitment lies in delivering exceptional care and unwavering support to our patients, guaranteeing their safety and successful recovery throughout their entire surgical experience.
Hospital Quality Awards
 America’s 50 Best Hospitals Award™ (2023, 2022)
America’s 50 Best Hospitals Award™ (2023, 2022)
Top 1% in the nation for providing the highest clinical quality year over year.

America’s 100 Best Hospitals Award™ (2021)
Top 2% in the nation for consistently delivering clinical quality year over year.

America’s 250 Best Hospitals Award™ (2023, 2022, 2021)
Top 5% in the nation for consistently delivering clinical quality.

Patient Safety Excellence Award™ (2023, 2022)
Top in the nation for providing excellence in patient safety by preventing infections, medical errors, and other preventable complications.
Specialty Clinical Quality Awards

America’s 100 Best Hospitals for Cardiac Care Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in heart bypass surgery, coronary interventional procedures, heart attack treatment, heart failure treatment, and heart valve surgery.

America’s 100 Best Hospitals for Coronary Intervention Award™ (2023, 2022, 2021, 2020, 2019)
Superior clinical outcomes in coronary intervention procedures (angioplasty with stent).

America’s 100 Best Hospitals for Prostate Surgery Award™ (2023, 2022, 2021)
Superior clinical outcomes in prostate removal surgery and transurethral resection of the prostate.
Click to see all of our Healthgrades best doctors awards
Visit our main website at www.LenoxHillMinimallyInvasiveSurgery.com
Blog Posts are Below:
Hernia Repair Surgery – NYC Surgeon
Hernia Repair Surgery: Steps, Benefits, Side-Effects, Precautions & Prognosis
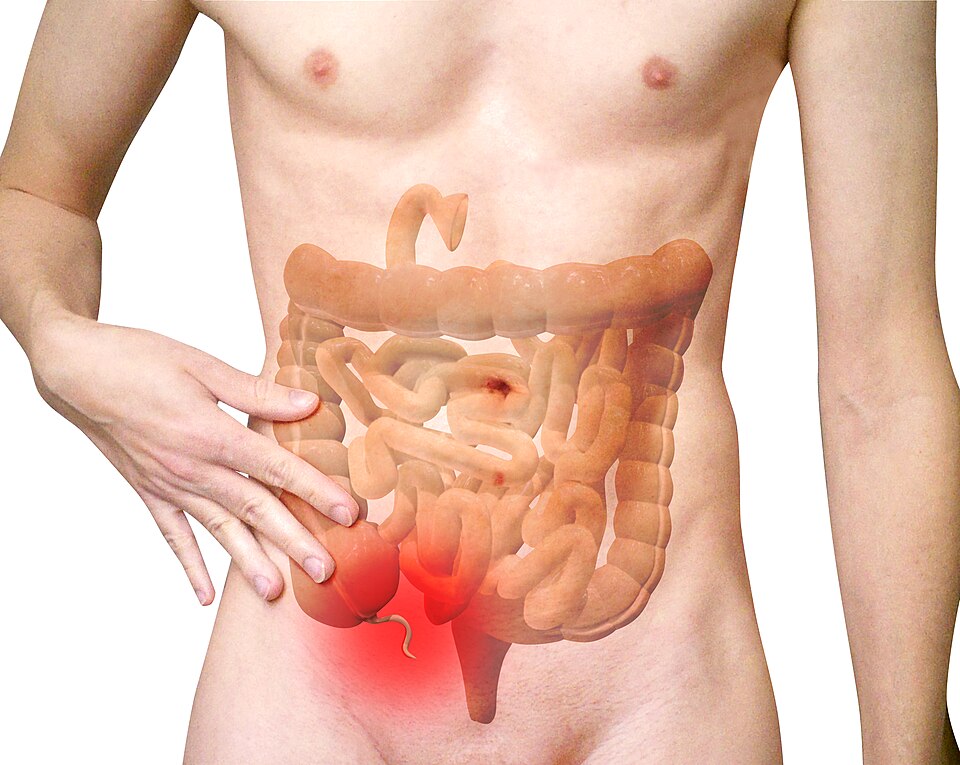
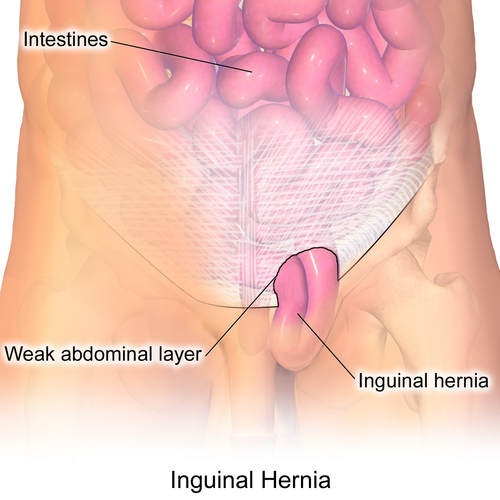
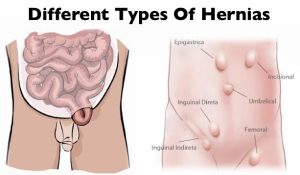 Hernia repair surgery entails the application of instrumental and manual procedures for correcting herniation of tissues or viscera including groin, abdomen, brain, and diaphragm. Internal organs, composed of tissues, could get herniated or bulged, forcing them to protrude via the wall encasing them. Hernias involving the groin (an inguinal hernia) and the umbilical cord (an umbilical hernia) are two of the most prevalent forms of a hernia.
Hernia repair surgery entails the application of instrumental and manual procedures for correcting herniation of tissues or viscera including groin, abdomen, brain, and diaphragm. Internal organs, composed of tissues, could get herniated or bulged, forcing them to protrude via the wall encasing them. Hernias involving the groin (an inguinal hernia) and the umbilical cord (an umbilical hernia) are two of the most prevalent forms of a hernia.
Since a hernia does not heal on its own but rather expands over time, it is crucial that you opt for surgical treatment to avoid unnecessary/preventable complications in the long run. Hernia surgery, usually performed on an outpatient basis, is a moderately simple operation that can help remedy the organ’s bulging and restore it to its original position.
Steps
 Two of the most popular types of hernia repair surgery is ‘herniorrhaphy’ and ‘hernioplasty’. Herniorrhaphy-the traditional hernia repair technique-is still conducted extensively where the surgeon makes a wide and long notch over the herniated organ. Thereafter, the physician removes the protrusion and reinstates the dislodged organ or tissues to its actual site.
Two of the most popular types of hernia repair surgery is ‘herniorrhaphy’ and ‘hernioplasty’. Herniorrhaphy-the traditional hernia repair technique-is still conducted extensively where the surgeon makes a wide and long notch over the herniated organ. Thereafter, the physician removes the protrusion and reinstates the dislodged organ or tissues to its actual site.
Finally, the doctor sutures the hole in the muscle via which the protuberance developed, sterilizes the incision, and sews it up. Hernioplasty is very much similar to herniorrhaphy procedurally excepting that in the final step, the surgeon overlays a sterile mesh (produced from animal tissues or polypropylene) on the muscular notch rather than suturing it. The nature or type of your herniation will determine the mode of repair surgery you’ll need to opt for.
Strangulated, reducible, and irreducible hernias are the three most widespread kinds of hernias. Both of the aforementioned surgical operation procedures can be carried out using a laparoscope or via open surgery.
Benefits
Both hernioplasty and herniorrhaphy are straightforward and uncomplicated surgical repair processes that take about 30-40 minutes to complete. You won’t feel any pain as the surgery will be done using either local or general anesthesia. Majority of patients are discharged from the hospital or medical center on the very day the laparoscopic surgery is performed. The usual benefits of the laparoscopic repair operation include:-
- Very short duration of stay
- Faster healing
- Reduced pain post surgery
- Quicker return to normal life
- Minimal costs (including all the expense heads)
- Lower risks of infection
Side Effects
The side effects of this type of surgery, most of which are rare, involve:-
- Swelling and redness around the incision or opening
- Blood clot
- Mesh pain
- Urinary tract infection
- Urinary incontinence
- Infection
- Difficulty urinating
- Hernia recurrence
- Neuralgia or nerve damage
- Constipation
- Kidney failure or complications
- Breathing problems or pneumonia
Precautions
You must abide by the surgeon’s instructions once you return home (which are usually on the same day the surgery is carried out) for a speedy recovery. Take all the prescribed medications on time, including the anti-inflammatory drugs for minimizing the possibilities of incision swelling. Contact your surgeon instantly if you’ve recurrent spells of fever, coughs, chills, nausea, abdominal swelling, bleeding as well as experience difficulty in urinating. Make sure you get sufficient rest for at least two weeks following the operation so that you can get back to work at the earliest.
Prognosis
Most hernia surgeries are effective, enabling patients to recover fully within 4-6 weeks. A typical person who has undergone hernia repair surgery can resume normal activities 2 weeks after the procedure.
Concluding Remarks
Opting for a surgical procedure for remedying a hernia is highly recommended not only for avoiding complications which could take a fatal turn (though very rare) but also for going back to leading a normal life. You can make an appointment with our general surgeon for a detailed, one-to-one consultation.
References
- http://www.medtronic.com/us-en/patients/treatments-therapies/hernia-surgery/about-recovery.html
- https://www.webmd.com/digestive-disorders/inguinal-hernia#1
- https://www.medicalnewstoday.com/articles/319753.php
- https://www.highgatehospital.co.uk/things-you-need-to-know-hernia-operation/
- https://www.webmd.com/digestive-disorders/need-surgery-hernia#1
- http://columbiasurgery.org/news/2014/04/15/hernias-what-you-need-know
- https://en.wikipedia.org/wiki/Hernia_repair
- https://my.clevelandclinic.org/health/treatments/6905-laparoscopic-surgery-for-hernia-repair/risks–benefits
General Surgery
Here are some brief descriptions about the different types of general surgery we perform:
Laparoscopic surgery
This is a relatively new specialty dealing with minimal access techniques using cameras and small instruments inserted through 0.3 to 1 cm incisions. Robotic surgery is now evolving from this concept (see below). Gallbladders, appendices, and colons can all be removed with this technique. Hernias are now repaired mostly laparoscopically. Most bariatric surgery is performed laparoscopically.[citation needed] General surgeons that are trained today are expected to be proficient in laparoscopic procedures.
Colorectal surgery
General surgeons treat a wide variety of major and minor colon and rectal diseases including inflammatory bowel diseases (such as ulcerative colitis or Crohn’s disease), diverticulitis, colon and rectal cancer, gastrointestinal bleeding and hemorrhoids.
Endocrine surgery
General surgeons are trained to remove all or part of the thyroid and parathyroid glands in the neck and the adrenal glands just above each kidney in the abdomen. In many communities, they are the only surgeon trained to do this. In communities that have a number of subspecialists, other subspecialty surgeons may assume responsibility for these procedures.
Surgical oncology
Surgical oncologist refers to a general surgical oncologist (a specialty of a general surgeon), but thoracic surgical oncologists, gynecologist and so forth can all be considered surgeons who specialize in treating cancer patients. The importance of training surgeons who sub-specialize in cancer surgery lies in evidence, supported by a number of clinical trials, that outcomes in surgical cancer care are positively associated to surgeon volume—i.e., the more cancer cases a surgeon treats, the more proficient he or she becomes, and his or her patients experience improved survival rates as a result. This is another controversial point, but it is generally accepted—even as common sense—that a surgeon who performs a given operation more often, will achieve superior results when compared with a surgeon who rarely performs the same procedure. This is particularly true of complex cancer resections such as pancreaticoduodenectomy for pancreatic cancer, and gastrectomy with extended (D2) lymphadenectomy for gastric cancer. Surgical oncology is generally a 2 year fellowship following completion of a general surgery residency (5-7 years).
Contact us at 646-846-1136 to schedule an appointment.
Robotic Surgery for General Surgical Procedures: Benefits and Innovations
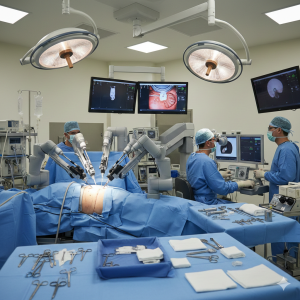 Robotic-assisted surgery has become he most exciting and transformative advancements for patients undergoing general surgical procedures. In NYC, robotic technology offers enhanced precision, reduced pain, and faster recovery compared to traditional open surgery. As innovation continues to evolve, robotic systems are redefining what’s possible in minimally invasive surgery.
Robotic-assisted surgery has become he most exciting and transformative advancements for patients undergoing general surgical procedures. In NYC, robotic technology offers enhanced precision, reduced pain, and faster recovery compared to traditional open surgery. As innovation continues to evolve, robotic systems are redefining what’s possible in minimally invasive surgery.
This guide explores how robotic surgery works, the procedures commonly performed, and why it has become a preferred option for many patients and surgeons.
What Is Robotic-Assisted Surgery?
Robotic surgery is a form of minimally invasive surgery in which the surgeon controls robotic arms from a console. The system translates the surgeon’s hand movements into smaller, more precise motions inside the body.
Contrary to common misconception:
- The robot does not operate independently.
- The surgeon is in full control at all times.
- The system enhances, rather than replaces, surgical skill.
Robotic platforms provide high-definition 3D visualization and instruments with a greater range of motion than the human wrist.
How Robotic Surgery Works
During the procedure:
- Small incisions (typically 5–10 mm) are made.
- A tiny camera provides magnified, 3D images of the surgical site.
- Robotic arms hold specialized instruments.
- The surgeon operates from a nearby console with precise control.
This advanced visualization and dexterity allow for delicate dissection and accurate suturing.
Common General Surgical Procedures Performed Robotically
Robotic-assisted techniques are now widely used in general surgery for:
- Hernia repair (inguinal, ventral, incisional)
- Colon and rectal surgery
- Gallbladder removal (cholecystectomy)
- GERD and hiatal hernia repair
- Adrenal gland surgery
- Pancreatic and liver procedures
- Complex reoperations with scar tissue
Robotic systems are particularly beneficial for complex abdominal and pelvic procedures where precision is critical.
Key Benefits of Robotic Surgery
1. Greater Precision
- Enhanced dexterity beyond natural wrist movement
- Elimination of hand tremors
- Fine control for delicate structures
2. Improved Visualization
- High-definition, 3D magnified view
- Better identification of nerves and blood vessels
- Improved accuracy in tumor removal
3. Smaller Incisions
- Less tissue trauma
- Reduced postoperative pain
- Minimal scarring
4. Faster Recovery
- Shorter hospital stays
- Earlier return to work and daily activities
- Lower risk of infection
For busy NYC patients, quicker recovery can mean minimal disruption to professional and personal life.
Robotic Surgery vs. Traditional Laparoscopy
While both robotic and laparoscopic procedures are minimally invasive, robotic surgery offers distinct advantages in certain cases.
- Robotic surgery provides 3D visualization, while traditional laparoscopy typically offers 2D imaging.
- Robotic instruments allow greater range of motion.
- Complex suturing and reconstruction are often easier robotically.
However, not every case requires robotic assistance. An experienced surgeon will determine the best approach based on the patient’s condition.
Innovations Driving the Future of Robotic Surgery
Robotic systems continue to evolve rapidly. Recent innovations include:
- Fluorescence imaging to assess blood flow in real time
- Enhanced energy devices for precise vessel sealing
- Improved instrument flexibility and control
- Advanced ergonomic consoles reducing surgeon fatigue
These technological advancements are improving patient safety and expanding the range of procedures that can be performed minimally invasively.
Who Is a Candidate for Robotic Surgery?
Most patients undergoing general surgery are candidates for robotic procedures, especially those with:
- Hernias requiring complex repair
- Colon conditions needing precise dissection
- GERD or hiatal hernias
- Previous abdominal surgeries with scar tissue
Patients with severe infection, unstable medical conditions, or extensive disease may require alternative approaches.
Are There Risks?
Robotic surgery is considered very safe, but like any procedure, it carries potential risks:
- Bleeding
- Infection
- Injury to surrounding organs
- Anesthesia-related complications
These risks are minimized when surgery is performed by a highly trained and experienced robotic surgeon.
Conclusion: The Future of General Surgery Is Here
Robotic-assisted surgery represents a major leap forward in general surgical care. By combining surgical expertise with advanced technology, patients benefit from greater precision, less pain, and faster recovery. In a city like NYC—where access to cutting-edge medical care is essential—robotic surgery provides an advanced solution for a wide range of procedures.
If you are considering surgery, ask whether a robotic-assisted approach may be right for you. Modern innovation is making surgery safer, more efficient, and more comfortable than ever before.
Contact Information
LENOX HILL MINIMALLY INVASIVE SURGERY LLP
155 East 76th Street
New York, NY 10021
Tel: 646-846-1136
Email: lenoxhillsurgeons@gmail.com
Visit us online: https://www.lenoxhillminimallyinvasivesurgery.com
Colon Surgery for Diverticulitis and Cancer: What to Expect
 Colon surgery is often recommended for patients suffering from recurrent diverticulitis or colon cancer. While the idea of colon surgery may feel overwhelming, modern minimally invasive techniques have made these procedures safer, more precise, and associated with faster recovery times. If you’ve been advised to undergo colon surgery in NYC, understanding what to expect can help you feel more confident and prepared.
Colon surgery is often recommended for patients suffering from recurrent diverticulitis or colon cancer. While the idea of colon surgery may feel overwhelming, modern minimally invasive techniques have made these procedures safer, more precise, and associated with faster recovery times. If you’ve been advised to undergo colon surgery in NYC, understanding what to expect can help you feel more confident and prepared.
This guide explains why colon surgery is performed, what the procedure involves, and how recovery typically progresses.
Understanding Diverticulitis and Colon Cancer
The colon (large intestine) plays a vital role in absorbing water and processing waste. When disease affects this organ, surgical intervention may be necessary.
Diverticulitis
Diverticulitis occurs when small pouches (diverticula) in the colon wall become inflamed or infected. While mild cases can be treated with antibiotics, surgery may be recommended if:
- You experience recurrent episodes
- Complications such as abscess, perforation, or fistula develop
- There is persistent pain or narrowing of the colon
Colon Cancer
Colon cancer develops when abnormal cells grow in the lining of the colon. Surgery is often the primary treatment, especially in early and mid-stage disease.
- Removal of the cancerous segment improves survival rates
- Lymph nodes are often removed for staging
- Surgery may be combined with chemotherapy depending on stage
Early detection through colonoscopy significantly improves outcomes.
What Is Colon Surgery?
Colon surgery, also known as colectomy or colon resection, involves removing the diseased portion of the colon and reconnecting the healthy ends.
There are different types of colon surgery depending on the location and severity of disease:
- Partial colectomy (removal of a segment of the colon)
- Right or left hemicolectomy (removal of one side of the colon)
- Sigmoid colectomy (commonly performed for diverticulitis)
- Total colectomy (removal of the entire colon, in rare cases)
Minimally Invasive Colon Surgery
In most cases today, colon surgery can be performed using laparoscopic or robotic-assisted techniques.
How It Works:
- Several small incisions are made in the abdomen
- A high-definition camera guides the surgeon
- The diseased portion of the colon is removed
- The healthy sections are reconnected (anastomosis)
Benefits:
- Smaller incisions and less scarring
- Reduced postoperative pain
- Shorter hospital stays
- Faster return to normal activities
- Lower risk of infection
Robotic surgery may provide additional precision, particularly in complex cancer cases.
Will I Need a Colostomy Bag?
One of the most common concerns patients have is whether they will need a colostomy (an opening in the abdomen for stool to exit into a bag).
- In most elective surgeries, reconnection is possible and no colostomy is needed.
- Temporary colostomies may be required in emergency situations or complicated infections.
- Permanent colostomies are uncommon and typically reserved for specific cancer cases.
Your surgeon will discuss this possibility with you before surgery.
Preparing for Colon Surgery
Before surgery, you may need:
- Bowel preparation (cleansing the colon)
- Blood tests and imaging
- Medication adjustments
- Preoperative consultation and clearance
Proper preparation helps reduce complications and supports smoother recovery.
What to Expect After Surgery
Hospital Stay
- Typically 2–5 days for minimally invasive surgery
- Longer stays may be needed for complicated cases
Recovery Timeline
- Walking is encouraged within 24 hours
- Diet progresses from liquids to solid foods gradually
- Return to work typically within 2–4 weeks
- Avoid heavy lifting for 4–6 weeks
Mild bloating, fatigue, and temporary bowel habit changes are common during early recovery.
Risks and Complications
Colon surgery is generally safe, but potential risks include:
- Infection
- Bleeding
- Anastomotic leak (rare but serious)
- Blood clots
- Bowel obstruction
Choosing an experienced minimally invasive surgeon significantly reduces these risks.
Long-Term Outlook
For diverticulitis patients, surgery often eliminates recurrent infections and dramatically improves quality of life.
For colon cancer patients, surgical removal of the tumor offers the best chance for cure, particularly when detected early. Follow-up care may include:
- Regular colonoscopies
- Imaging scans
- Blood work
- Oncology consultations if needed
Conclusion: Modern Colon Surgery Offers Hope and Healing
Colon surgery for diverticulitis and cancer has advanced significantly, offering safer procedures and quicker recovery thanks to minimally invasive techniques. If you are experiencing recurrent diverticulitis or have been diagnosed with colon cancer, timely surgical consultation can provide clarity and effective treatment options.
Contact Information
LENOX HILL MINIMALLY INVASIVE SURGERY PLLC
Dr. Valery Dronsky
117 E 77th Street
New York, NY 10075
646-846-1136
admin@lenoxmis.com
Visit us online:
https://www.lenoxhillminimallyinvasivesurgery.com
Minimally Invasive Surgery in NYC: Faster Recovery, Less Pain
 Minimally invasive surgery in large cities like NYC has revolutionized the way many common and complex procedures are performed. For patients in New York City, where busy schedules and active lifestyles are the norm, choosing a surgical approach that allows for faster recovery and less pain is often a top priority. Thanks to advances in laparoscopic and robotic-assisted techniques, minimally invasive surgery (MIS) offers safer, more efficient solutions for a wide range of general surgical conditions.
Minimally invasive surgery in large cities like NYC has revolutionized the way many common and complex procedures are performed. For patients in New York City, where busy schedules and active lifestyles are the norm, choosing a surgical approach that allows for faster recovery and less pain is often a top priority. Thanks to advances in laparoscopic and robotic-assisted techniques, minimally invasive surgery (MIS) offers safer, more efficient solutions for a wide range of general surgical conditions.
This guide explains how minimally invasive surgery works, its benefits, and why it has become the preferred option for many patients in NYC.
What Is Minimally Invasive Surgery?
Minimally invasive surgery refers to procedures performed through small incisions using specialized instruments and high-definition cameras. Instead of making a large incision as in traditional open surgery, surgeons use tools such as laparoscopes or robotic systems to operate with precision while minimizing trauma to surrounding tissues.
Common minimally invasive techniques include:
- Laparoscopic surgery
- Robotic-assisted surgery
- Single-incision laparoscopic surgery (SILS)
- Advanced endoscopic procedures
These approaches are now widely used across general surgery, offering patients significant advantages over conventional methods.
Key Benefits: Faster Recovery and Less Pain
The primary reasons patients choose minimally invasive surgery are the reduced recovery time and lower levels of postoperative discomfort.
- Smaller incisions: Less tissue damage leads to decreased pain and quicker healing.
- Shorter hospital stays: Many procedures are outpatient or require only overnight observation.
- Reduced need for pain medication: Patients often require fewer narcotics after surgery.
- Faster return to normal activities: Many individuals resume work and daily routines within 1–2 weeks.
- Lower risk of infection: Smaller wounds decrease the likelihood of surgical site infections.
- Minimal scarring: Cosmetic outcomes are significantly improved.
For NYC residents balancing work, commuting, and family life, this accelerated recovery can make a substantial difference.
Conditions Commonly Treated with Minimally Invasive Surgery
Minimally invasive techniques are used to treat many of the most common general surgical conditions.
- Hernias (inguinal, umbilical, ventral, incisional)
- Gallbladder disease and gallstones
- Appendicitis
- Colon and small intestine disorders
- GERD and hiatal hernias
- Adrenal gland tumors
- Liver and pancreatic conditions
- Soft tissue masses and skin lesions
In most cases, patients experience fewer complications and shorter recovery periods compared to traditional open surgery.
Laparoscopic vs. Robotic Surgery
Both laparoscopic and robotic-assisted procedures fall under the umbrella of minimally invasive surgery, but they offer slightly different advantages.
Laparoscopic Surgery
- Uses small incisions and a camera to guide surgical instruments
- Well-established and widely used
- Effective for most routine procedures
Robotic-Assisted Surgery
- Provides enhanced 3D visualization
- Allows for greater precision and dexterity
- Particularly beneficial for complex or delicate operations
Your surgeon will determine which approach is best based on your specific condition and overall health.
What to Expect Before and After Surgery
Before surgery, you will undergo a thorough evaluation including imaging, lab tests, and a consultation to determine your candidacy for a minimally invasive approach.
After surgery:
- You may go home the same day
- Mild soreness or bloating is common
- Light activity is encouraged within days
- Heavy lifting is typically restricted for several weeks
Most patients are surprised by how quickly they regain energy and mobility.
Is Minimally Invasive Surgery Right for You?
While most patients are candidates for minimally invasive surgery, certain factors may influence the decision:
- Previous abdominal surgeries causing scar tissue
- Severe infection or inflammation
- Complex anatomy or advanced disease
- Underlying medical conditions
An experienced surgeon will evaluate your individual situation to determine the safest and most effective treatment plan.
Why NYC Patients Prefer Minimally Invasive Surgery
Living in NYC means balancing demanding careers, family commitments, and an active lifestyle. Minimally invasive surgery allows patients to:
- Return to work sooner
- Avoid prolonged hospital stays
- Minimize disruption to daily routines
- Heal comfortably and discreetly
Access to advanced surgical technology and experienced specialists makes NYC one of the best places to undergo minimally invasive procedures.
Conclusion: Advanced Care with Faster Healing
Minimally invasive surgery represents the future of general surgical care. With faster recovery, less pain, and lower complication rates, it has become the preferred option for many procedures. If you’re facing surgery, exploring minimally invasive options could significantly improve your experience and outcome.
Contact Information
LENOX HILL MINIMALLY INVASIVE SURGERY PLLC
Dr. Valery Dronsky
117 E 77th Street
New York, NY 10075
646-846-1136
admin@lenoxmis.com
Visit us online: https://www.lenoxhillminimallyinvasivesurgery.com
Appendectomy Explained: What NYC Patients Should Know About Appendix Surgery
What is appendix surgery? Appendicitis is one of the most common surgical emergencies in the United States. When the appendix becomes inflamed or infected, prompt surgical removal—called an appendectomy—is typically required to prevent serious complications. For patients in New York City, understanding the symptoms, treatment options, and recovery expectations can make a stressful situation much more manageable.
This guide explains everything NYC patients should know about appendix surgery, from diagnosis to recovery.
What Is the Appendix?
The appendix is a small, tube-shaped organ located in the lower right side of the abdomen. While its exact function is not fully understood, it is not considered essential for normal digestion.
However, when the appendix becomes blocked or infected, it can quickly lead to a dangerous condition known as appendicitis.
What Causes Appendicitis?
Appendicitis typically occurs when the appendix becomes obstructed, leading to inflammation and infection.
- Blockage from hardened stool (fecalith)
- Bacterial or viral infection
- Swollen lymph tissue
- Rarely, tumors or foreign bodies
If untreated, the appendix can rupture, spreading infection throughout the abdomen (a condition called peritonitis), which can be life-threatening.
Common Symptoms of Appendicitis
Recognizing the symptoms early is critical. Classic signs include:
- Sudden pain that begins near the belly button and shifts to the lower right abdomen
- Worsening pain with movement, coughing, or pressure
- Nausea and vomiting
- Loss of appetite
- Low-grade fever
- Abdominal bloating
- Difficulty passing gas
In NYC’s fast-paced environment, many people delay seeking care—but appendicitis requires urgent medical evaluation.
How Is Appendicitis Diagnosed?
Diagnosis usually involves:
- Physical examination: Checking for tenderness in the lower right abdomen
- Blood tests: Elevated white blood cell count indicating infection
- Imaging studies: CT scan or ultrasound to confirm inflammation
Early and accurate diagnosis allows for safer, minimally invasive treatment.
What Is an Appendectomy?
An appendectomy is the surgical removal of the appendix. It is one of the most commonly performed emergency procedures.
There are two main approaches:
1. Laparoscopic Appendectomy (Minimally Invasive)
This is the preferred method in most cases.
- Several small incisions are made in the abdomen
- A tiny camera (laparoscope) guides the procedure
- The appendix is removed using specialized instruments
- Patients often go home the same day or within 24 hours
Benefits:
- Less pain
- Minimal scarring
- Shorter hospital stay
- Faster return to work and daily activities
2. Open Appendectomy
In cases of rupture or severe infection, an open procedure may be necessary.
- A larger incision is made in the lower right abdomen
- The infected appendix is removed directly
- The abdominal cavity may be cleaned if infection has spread
Open surgery typically involves a slightly longer recovery period.
Is Appendectomy Always Necessary?
In certain mild cases, antibiotics may temporarily treat appendicitis. However:
- There is a higher chance of recurrence
- Delayed surgery increases risk of rupture
- Surgery remains the definitive treatment
Most surgeons recommend appendectomy to eliminate future risk.
What to Expect After Appendix Surgery
Recovery depends on whether the appendix ruptured and which surgical method was used.
After Laparoscopic Surgery:
- Return home within 24 hours
- Resume light activity within a few days
- Return to work in 1–2 weeks
- Avoid heavy lifting for 2–4 weeks
After Open Surgery:
- Hospital stay of 2–3 days if infection was present
- Return to work in 2–4 weeks
- Longer activity restrictions
Pain is usually manageable with prescribed or over-the-counter medications.
Potential Complications
Appendectomy is generally very safe, but possible complications include:
- Wound infection
- Abscess formation
- Bleeding
- Adverse reaction to anesthesia
Choosing an experienced surgical team significantly reduces these risks.
Living Without an Appendix
The good news: you can live completely normally without your appendix. There are no long-term dietary restrictions or lifestyle limitations after recovery.
Why Prompt Treatment Matters in NYC
In a city like New York, access to advanced surgical care is readily available. Delaying care due to busy schedules can increase the risk of rupture and complications. Seeking immediate medical attention when symptoms arise leads to:
- Lower complication rates
- Faster recovery
- Reduced hospital stays
- Better overall outcomes
Conclusion: Act Quickly for the Best Outcome
Appendicitis is a medical emergency that requires timely surgical treatment. Fortunately, modern minimally invasive appendectomy techniques allow for quick recovery and excellent outcomes. If you experience symptoms of appendicitis, don’t ignore them—early intervention is key.
If you are in NYC and need expert evaluation or emergency surgical care, the experienced team at Lenox Hill Minimally Invasive Surgery PLLC is ready to provide advanced, compassionate treatment.
Contact Information
LENOX HILL MINIMALLY INVASIVE SURGERY PLLC
Dr. Valery Dronsky
117 E 77th Street
New York, NY 10075
646-846-1136
admin@lenoxmis.com
Visit us online: https://www.lenoxhillminimallyinvasivesurgery.com
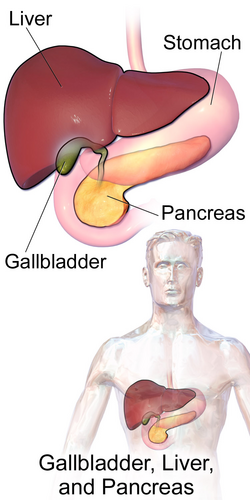
Gallbladder Surgery in NYC: Is Laparoscopic Cholecystectomy Right for You?
Thanks to modern advances, the most common and effective method today for gallbladder removal surgery is laparoscopic cholecystectomy—a minimally invasive approach offering faster recovery and less pain. Gallbladder issues, such as gallstones or inflammation, can cause persistent abdominal pain and digestive disturbances. If you’ve been diagnosed with gallbladder disease and conservative treatments haven’t worked, your doctor may recommend gallbladder removal surgery, known as a cholecystectomy.
If you’re considering gallbladder surgery in NYC, this guide will help you understand whether laparoscopic cholecystectomy is the right choice for you.

What Is the Gallbladder and Why Is It Removed?
The gallbladder is a small, pear-shaped organ located beneath the liver. It stores bile—a digestive fluid produced by the liver—and releases it into the small intestine to help break down fats.
However, the gallbladder isn’t essential to digestion. When it becomes diseased or develops stones that block bile flow, removing it is often the most effective solution.
Common Conditions Requiring Gallbladder Surgery
Gallbladder removal may be recommended for:
- Gallstones (cholelithiasis): Hardened deposits of bile that can block ducts and cause pain
- Cholecystitis: Inflammation of the gallbladder, often due to gallstones
- Biliary dyskinesia: Poor function of the gallbladder leading to chronic pain
- Gallbladder polyps or tumors: Abnormal growths requiring removal for further evaluation
- Pancreatitis due to gallstones: Inflammation of the pancreas triggered by a blocked bile duct
If these conditions cause ongoing pain, nausea, vomiting, or digestion problems, surgery is typically the most effective treatment.
What Is Laparoscopic Cholecystectomy?
Laparoscopic cholecystectomy is a minimally invasive procedure to remove the gallbladder using small incisions and a tiny camera called a laparoscope. It has become the standard approach for gallbladder removal due to its safety and faster recovery.
Procedure Overview:
- Four small incisions (usually under 1 inch each) are made in the abdomen
- A laparoscope provides high-definition imaging to guide the surgeon
- Special instruments are used to detach and remove the gallbladder
- The incisions are closed with sutures or surgical glue
- Most patients go home the same day
Benefits of Laparoscopic Gallbladder Surgery
Compared to open surgery, laparoscopic cholecystectomy offers several key advantages:
- Less postoperative pain
- Shorter hospital stay (often outpatient)
- Faster return to normal activities (usually within 1–2 weeks)
- Smaller scars and improved cosmetic outcomes
- Lower risk of infection and complications
This approach is particularly well-suited for patients in busy urban settings like NYC, where a faster recovery can mean less time off work or away from family responsibilities.
Who Is a Candidate for Laparoscopic Cholecystectomy?
Most patients diagnosed with gallbladder disease are eligible for laparoscopic surgery. However, certain factors may affect your candidacy:
- Previous abdominal surgeries causing scar tissue
- Severe inflammation or infection (may require open surgery)
- Bleeding disorders or other high-risk medical conditions
- Pregnancy (in select cases, surgery may still be performed safely)
Your surgeon will conduct a full evaluation to determine the safest and most effective approach for your condition.
What to Expect During Recovery
Recovery after laparoscopic gallbladder removal is generally smooth and quick.
- Most patients return home within a few hours after surgery
- Light activities can resume within a few days
- Most people return to work within 1–2 weeks
- You may experience mild bloating or soreness near the incision sites
- Dietary adjustments may be recommended to ease digestion initially
Follow-up appointments help ensure proper healing and monitor for any complications.
Are There Any Risks or Complications?
Laparoscopic cholecystectomy is a safe and commonly performed procedure, but like all surgeries, it carries some risks, including:
- Bleeding or infection
- Bile duct injury (rare)
- Reaction to anesthesia
- Residual bile duct stones requiring further treatment
These risks are minimized when the procedure is performed by an experienced surgeon in a well-equipped facility.
Conclusion: Is Laparoscopic Cholecystectomy Right for You?
If you’re suffering from gallstones or gallbladder inflammation, laparoscopic cholecystectomy may be your best path to lasting relief. It’s safe, effective, and minimally disruptive—especially when performed by a skilled surgical team in NYC.
Don’t wait for your symptoms to worsen. Early evaluation and timely treatment can prevent serious complications and help you return to a pain-free, healthy lifestyle.
Contact Information
LENOX HILL MINIMALLY INVASIVE SURGERY LLP
155 East 76th Street
New York, NY 10021
Tel: 646-846-1136
Email: lenoxhillsurgeons@gmail.com
Umbilical and Incisional Hernias: When Is Surgery Necessary?
Hernias can develop in various parts of the abdominal wall, and two of the most frequently encountered types are umbilical hernias and incisional hernias. While both involve a bulge or protrusion of tissue through a weakened area in the abdominal muscles, their causes and treatment approaches differ. Understanding when surgery is necessary for these types of hernias is essential to prevent complications and ensure long-term health.
This guide will help you recognize the signs, understand the risks, and explore the surgical options available for umbilical and incisional hernias—especially using modern minimally invasive techniques.
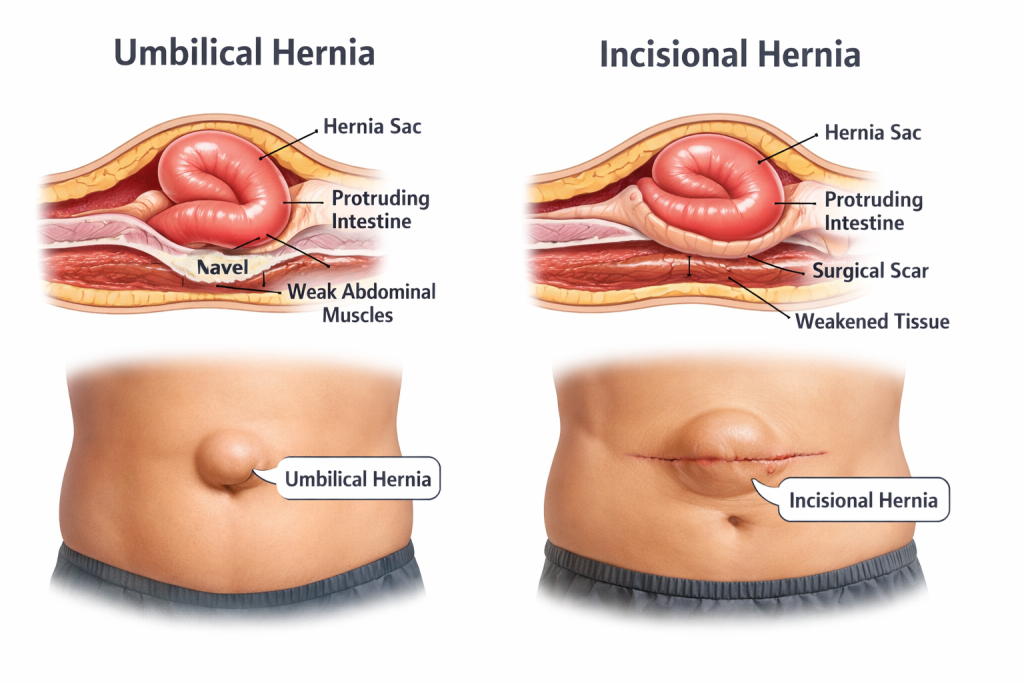
What Is an Umbilical Hernia?
An umbilical hernia occurs when part of the intestine or fatty tissue protrudes through the abdominal wall near the belly button (umbilicus). This type of hernia is common in infants but also affects adults, particularly women who have experienced multiple pregnancies or people who are overweight.
Common Causes:
- Congenital weakness in the abdominal wall
- Pregnancy or multiple pregnancies
- Obesity and weight gain
- Heavy lifting or straining
In adults, umbilical hernias are less likely to resolve on their own and often require surgical correction.
What Is an Incisional Hernia?
An incisional hernia develops at the site of a previous surgical incision where the abdominal wall hasn’t fully healed. This type of hernia can occur weeks, months, or even years after surgery.
Risk Factors:
- Infection or poor wound healing after initial surgery
- Obesity or excessive strain on the surgical site
- Multiple abdominal surgeries
- Smoking or chronic diseases that impair healing
Incisional hernias can become large and uncomfortable, often requiring surgical repair to restore function and prevent complications.
Signs and Symptoms of Both Hernia Types
Regardless of the type, umbilical and incisional hernias tend to present with similar symptoms:
- A visible bulge near the belly button or previous surgical site
- Pain or pressure, especially when lifting, bending, or coughing
- A feeling of weakness or heaviness in the abdominal wall
- Redness, swelling, or tenderness in the hernia area (especially if strangulated)
- Nausea or vomiting if intestinal obstruction is present
If the hernia cannot be pushed back in or causes severe pain and discoloration, this could indicate strangulation—a serious condition requiring emergency surgery.
When Is Surgery Necessary?
Not all hernias require immediate surgery, but several factors make surgical repair the best option:
- The hernia is growing or becoming more painful
- Daily activities are impacted by discomfort or pressure
- There’s a risk of incarceration (trapped tissue) or strangulation (cut-off blood supply)
- The hernia is irreducible (cannot be pushed back in)
- Cosmetic or lifestyle concerns motivate the patient to seek repair
In adults, umbilical hernias rarely close on their own. Similarly, incisional hernias do not improve without intervention and often worsen over time.
Surgical Options: Open vs. Minimally Invasive Repair
There are two primary surgical techniques for repairing umbilical and incisional hernias:
1. Open Hernia Repair
- Traditional approach with a single incision over the hernia site
- Surgeon returns the protruding tissue to the abdomen and closes the defect, often using mesh for reinforcement
- May be recommended for large or complex hernias
2. Laparoscopic or Robotic-Assisted Hernia Repair
- Minimally invasive approach using several small incisions and a camera
- Surgeon places mesh from the inside to reinforce the abdominal wall
- Offers faster recovery, less post-operative pain, and lower infection risk
Your surgeon will recommend the best approach based on the hernia’s size, location, your medical history, and lifestyle.
Recovery After Surgery
Most patients return home the same day, especially with laparoscopic surgery. Recovery tips include:
- Avoid lifting heavy objects for at least 4–6 weeks
- Follow a high-fiber diet to prevent straining during bowel movements
- Monitor for signs of infection or recurrence
- Gradually increase activity as advised by your surgeon
Follow-up visits are essential to monitor healing and ensure the hernia repair is successful.
Conclusion: Don’t Delay Hernia Evaluation
Umbilical and incisional hernias can seem minor at first but tend to worsen over time. If you’re experiencing bulging, discomfort, or pressure in your abdominal area, it’s important to seek a professional evaluation. Minimally invasive surgical techniques make hernia repair safer and more efficient than ever, with less downtime and improved outcomes.
Contact Information
LENOX HILL MINIMALLY INVASIVE SURGERY LLP
155 East 76th Street
New York, NY 10021
Tel: 646-846-1136
Email: lenoxhillsurgeons@gmail.com
Understanding Inguinal Hernias: Causes, Symptoms, and Surgical Options
Inguinal hernias are among the most common types of hernias, particularly affecting men. They occur when a portion of the intestine or abdominal tissue protrudes through a weakened area in the lower abdominal wall, often near the inguinal canal. While some inguinal hernias may cause minimal discomfort initially, they can enlarge over time and lead to serious complications if left untreated.
This guide explores the causes, symptoms, diagnosis, and treatment options for inguinal hernias, especially the benefits of surgical repair using minimally invasive techniques.
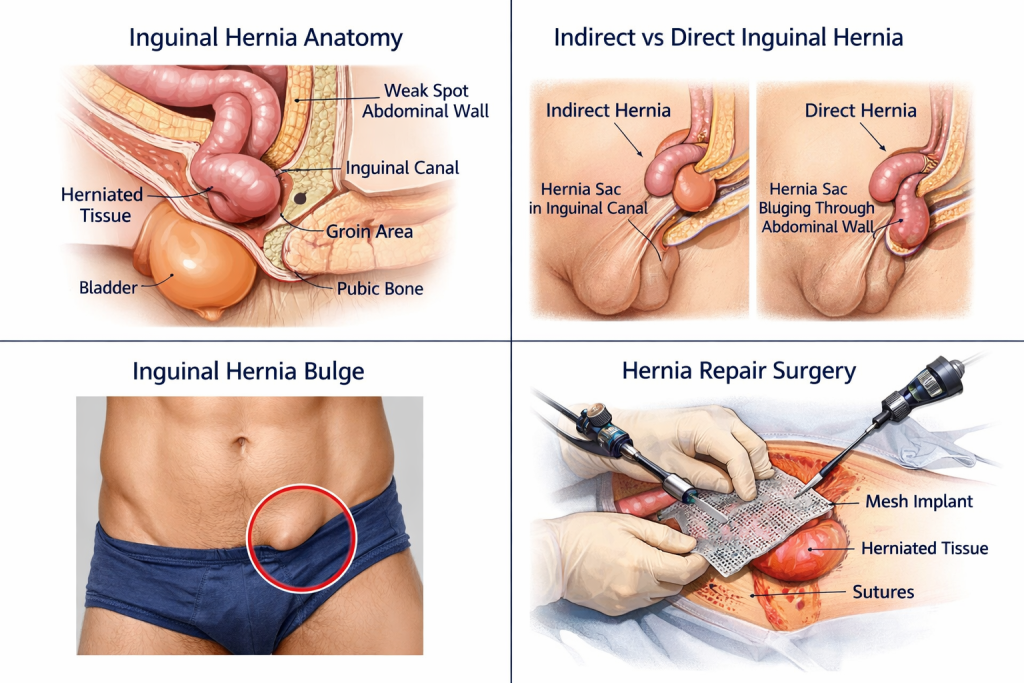
What Causes an Inguinal Hernia?
Inguinal hernias develop when the muscles of the abdominal wall weaken or experience increased pressure, allowing internal tissue to push through.
- Congenital defects: Some people are born with a weakness in the abdominal wall that makes them more susceptible to hernias.
- Chronic straining: Straining from heavy lifting, persistent coughing, or constipation increases pressure inside the abdomen.
- Aging: Muscle strength naturally decreases with age, making older adults more vulnerable to hernias.
- Obesity: Excess body weight adds pressure on the abdominal muscles, contributing to hernia formation.
- Previous surgeries: Surgical incisions or scar tissue may weaken the abdominal wall, allowing hernias to develop.
Men are significantly more likely to develop inguinal hernias than women, due to anatomical differences and the presence of the spermatic cord passing through the inguinal canal.
Recognizing the Symptoms of an Inguinal Hernia
Symptoms of an inguinal hernia can range from mild to severe and may include:
- A noticeable bulge on one or both sides of the groin, which becomes more prominent when standing or straining
- Discomfort, heaviness, or aching in the groin area
- Pain when coughing, bending over, or lifting heavy objects
- Burning or pressure in the groin
- Swelling around the testicles in men, if the hernia descends into the scrotum
In some cases, the hernia may be reducible—meaning it can be gently pushed back into the abdomen. However, a strangulated hernia (where blood supply is cut off) is a medical emergency and may present with:
- Sudden, intense groin pain
- Redness or discoloration of the bulge
- Fever or nausea
- Inability to pass gas or have a bowel movement
If these symptoms occur, immediate surgical attention is required.
How Inguinal Hernias Are Diagnosed
A diagnosis is typically made through a physical examination. During the exam, the surgeon may ask you to stand and cough to make the hernia more visible. Imaging studies, such as an ultrasound or CT scan, may be used to confirm the diagnosis or assess the hernia’s size and contents.
Treatment Options for Inguinal Hernias
While small, asymptomatic hernias may be monitored, surgery is the definitive treatment for inguinal hernias. Surgical repair is recommended for:
- Persistent pain or discomfort
- Rapidly enlarging hernia
- Impairment in daily activities
- Risk of complications like incarceration or strangulation
Surgical Approaches
There are two main types of hernia repair surgery:
- Open hernia repair: A single incision is made in the groin to push the protruding tissue back and reinforce the abdominal wall with mesh.
- Laparoscopic or robotic-assisted repair: Multiple small incisions are used to insert a camera and instruments. The hernia is repaired from inside the abdomen using mesh reinforcement.
Minimally invasive techniques offer several advantages:
- Smaller incisions and less scarring
- Reduced postoperative pain
- Shorter recovery time and faster return to normal activities
- Lower risk of infection and complications
Your surgeon will determine the best approach based on your medical history, the size and type of hernia, and overall health.
Recovery After Inguinal Hernia Surgery
Most patients recover quickly after minimally invasive hernia repair. Common post-op recommendations include:
- Light activity within a few days
- Avoiding heavy lifting for 4–6 weeks
- Using over-the-counter or prescribed pain medication as needed
- Monitoring for signs of infection or recurrence
Follow-up appointments help ensure proper healing and assess for any complications.
Conclusion: Don’t Ignore the Signs of a Hernia
Inguinal hernias are common and often manageable, but they do not resolve on their own. If you suspect you have a hernia, it’s essential to seek evaluation from an experienced general surgeon. With today’s advanced surgical options, most patients experience excellent outcomes and can return to their daily routines with confidence and comfort.
Contact Information
LENOX HILL MINIMALLY INVASIVE SURGERY LLP
155 East 76th Street
New York, NY 10021
Tel: 646-846-1136
Email: lenoxhillsurgeons@gmail.com
Visit us online: https://www.lenoxhillminimallyinvasivesurgery.com
The Benefits of Having Surgery at a New York City Practice
 Here we will explore the nuances of the benefits of having surgery at a new york city practice and what patients need to know. Surgical procedures are a critical component of modern medicine, addressing a wide range of health concerns. Whether you’re preparing for surgery or considering your options, understanding the process and the latest advancements can help you make informed decisions.
Here we will explore the nuances of the benefits of having surgery at a new york city practice and what patients need to know. Surgical procedures are a critical component of modern medicine, addressing a wide range of health concerns. Whether you’re preparing for surgery or considering your options, understanding the process and the latest advancements can help you make informed decisions.
Why Surgery is Recommended
Surgery can address a variety of medical issues, from life-saving interventions to elective procedures that improve quality of life. It’s important for patients to understand why their doctor may recommend surgery and what outcomes they can expect.
How to Prepare for a Medical Procedure
- Know Your Procedure: Researching the specific type of surgery you’re undergoing helps reduce anxiety and allows you to ask informed questions during consultations.
- Follow Preoperative Instructions: Surgeons typically provide guidelines such as fasting before surgery or adjusting medications. Adhering to these instructions is crucial for safety.
- Plan for Recovery: Consider who will assist you after surgery, whether it’s arranging transportation or having someone help with daily tasks during your recovery period.
The Advantages of Minimally Invasive Surgery
Minimally invasive surgery has revolutionized how procedures are performed, offering patients faster recovery times and fewer complications. These techniques often involve smaller incisions, reduced scarring, and a quicker return to normal activities.
The Role of Regular Health Screenings
Screening is a cornerstone of preventive healthcare. Procedures like colonoscopies can detect issues such as polyps or colorectal cancer early, significantly improving treatment outcomes. Regular health check-ups and open communication with your healthcare provider are essential for staying proactive about your health.
Steps for a Quick Recovery
Recovering from surgery requires patience and adherence to your doctor’s recommendations. Here are some general tips to ensure a smooth recovery:
- Follow Discharge Instructions: Carefully read and follow the post-operative care guidelines provided by your surgeon.
- Stay Active (But Don’t Overdo It): Gentle movement, as recommended, can help prevent blood clots and improve healing.
- Eat a Balanced Diet: Proper nutrition supports your body’s recovery process, promoting faster healing.
Key Questions to Ask Before Surgery
Before undergoing any surgical procedure, it’s important to have a thorough discussion with your surgeon. Key topics to cover include:
- The risks and benefits of the procedure.
- What to expect during the recovery period.
- Alternative treatments, if available.

Benefits of Having Surgery at a New York City Practice: Contact Us Today
Surgery in NYC has never been more accessible. Contact Lenox Hill Minimally Invasive Surgery LLP for expert care tailored to your needs.
LENOX HILL MINIMALLY INVASIVE SURGERY LLP
155 East 76th Street
New York, NY 10021
Tel: 646-846-1136
Email: lenoxhillsurgeons@gmail.com
Addressing Colorectal Health: Procedures and Prevention
This blog explores the nuances of addressing colorectal health procedures and prevention and what patients need to know. Surgical procedures are a critical component of modern medicine, addressing a wide range of health concerns. Whether you’re preparing for surgery or considering your options, understanding the process and the latest advancements can help you make informed decisions.
Exploring the Need for Surgery
Surgery can address a variety of medical issues, from life-saving interventions to elective procedures that improve quality of life. It’s important for patients to understand why their doctor may recommend surgery and what outcomes they can expect.
Getting Ready for Your Operation
- Know Your Procedure: Researching the specific type of surgery you’re undergoing helps reduce anxiety and allows you to ask informed questions during consultations.
- Follow Preoperative Instructions: Surgeons typically provide guidelines such as fasting before surgery or adjusting medications. Adhering to these instructions is crucial for safety.
- Plan for Recovery: Consider who will assist you after surgery, whether it’s arranging transportation or having someone help with daily tasks during your recovery period.
Revolutionary Minimally Invasive Options
Minimally invasive surgery has revolutionized how procedures are performed, offering patients faster recovery times and fewer complications. These techniques often involve smaller incisions, reduced scarring, and a quicker return to normal activities.
How Early Detection Impacts Surgery
Screening is a cornerstone of preventive healthcare. Procedures like colonoscopies can detect issues such as polyps or colorectal cancer early, significantly improving treatment outcomes. Regular health check-ups and open communication with your healthcare provider are essential for staying proactive about your health.
Nutrition and Exercise After Surgery
Recovering from surgery requires patience and adherence to your doctor’s recommendations. Here are some general tips to ensure a smooth recovery:
- Follow Discharge Instructions: Carefully read and follow the post-operative care guidelines provided by your surgeon.
- Stay Active (But Don’t Overdo It): Gentle movement, as recommended, can help prevent blood clots and improve healing.
- Eat a Balanced Diet: Proper nutrition supports your body’s recovery process, promoting faster healing.
Understanding Surgical Risks and Alternatives
Before undergoing any surgical procedure, it’s important to have a thorough discussion with your surgeon. Key topics to cover include:
- The risks and benefits of the procedure.
- What to expect during the recovery period.
- Alternative treatments, if available.
Colorectal Health Procedures and Prevention: Contact Us Today
Lenox Hill Minimally Invasive Surgery LLP specializes in colorectal procedures that prioritize your health and well-being.
Call us to schedule your consultation.
LENOX HILL MINIMALLY INVASIVE SURGERY LLP
155 East 76th Street
New York, NY 10021
Tel: 646-846-1136
Email: lenoxhillsurgeons@gmail.com
Common Questions About Gallbladder Surgery Answered
 This blog explores the nuances of common questions about gallbladder surgery answered and what patients need to know. Surgical procedures are a critical component of modern medicine, addressing a wide range of health concerns. Whether you’re preparing for surgery or considering your options, understanding the process and the latest advancements can help you make informed decisions.
This blog explores the nuances of common questions about gallbladder surgery answered and what patients need to know. Surgical procedures are a critical component of modern medicine, addressing a wide range of health concerns. Whether you’re preparing for surgery or considering your options, understanding the process and the latest advancements can help you make informed decisions.
What Makes a Procedure Necessary
Surgery can address a variety of medical issues, from life-saving interventions to elective procedures that improve quality of life. It’s important for patients to understand why their doctor may recommend surgery and what outcomes they can expect.
Preparation Tips for Better Surgical Outcomes
- Know Your Procedure: Researching the specific type of surgery you’re undergoing helps reduce anxiety and allows you to ask informed questions during consultations.
- Follow Preoperative Instructions: Surgeons typically provide guidelines such as fasting before surgery or adjusting medications. Adhering to these instructions is crucial for safety.
- Plan for Recovery: Consider who will assist you after surgery, whether it’s arranging transportation or having someone help with daily tasks during your recovery period.
Advancements in Surgical Techniques
Minimally invasive surgery has revolutionized how procedures are performed, offering patients faster recovery times and fewer complications. These techniques often involve smaller incisions, reduced scarring, and a quicker return to normal activities.
Screenings That Can Save Lives
Screening is a cornerstone of preventive healthcare. Procedures like colonoscopies can detect issues such as polyps or colorectal cancer early, significantly improving treatment outcomes. Regular health check-ups and open communication with your healthcare provider are essential for staying proactive about your health.
Effective Recovery Strategies
Recovering from surgery requires patience and adherence to your doctor’s recommendations. Here are some general tips to ensure a smooth recovery:
- Follow Discharge Instructions: Carefully read and follow the post-operative care guidelines provided by your surgeon.
- Stay Active (But Don’t Overdo It): Gentle movement, as recommended, can help prevent blood clots and improve healing.
- Eat a Balanced Diet: Proper nutrition supports your body’s recovery process, promoting faster healing.
Talking with Your Surgeon About Your Concerns
Before undergoing any surgical procedure, it’s important to have a thorough discussion with your surgeon. Key topics to cover include:
- The risks and benefits of the procedure.
- What to expect during the recovery period.
- Alternative treatments, if available.
Questions About Gallbladder Surgery? Contact Us Today
Do you have questions about gallbladder surgery? Lenox Hill Minimally Invasive Surgery LLP is here to provide answers and exceptional care. Contact us today!
LENOX HILL MINIMALLY INVASIVE SURGERY LLP
155 East 76th Street
New York, NY 10021
Tel: 646-846-1136
Email: lenoxhillsurgeons@gmail.com
Lenox Hill Minimally Invasive Surgery: Expertise in Hernia Repair Surgery
Let’s explore the nuances of lenox hill minimally invasive surgery’s expertise in hernia repair surgery and what patients need to know. Surgical procedures are a critical component of modern medicine, addressing a wide range of health concerns. Whether you’re preparing for surgery or considering your options, understanding the process and the latest advancements can help you make informed decisions.
Why Surgery is Recommended
Surgery can address a variety of medical issues, from life-saving interventions to elective procedures that improve quality of life. It’s important for patients to understand why their doctor may recommend surgery and what outcomes they can expect.
How to Prepare for a Medical Procedure
- Know Your Procedure: Researching the specific type of surgery you’re undergoing helps reduce anxiety and allows you to ask informed questions during consultations.
- Follow Preoperative Instructions: Surgeons typically provide guidelines such as fasting before surgery or adjusting medications. Adhering to these instructions is crucial for safety.
- Plan for Recovery: Consider who will assist you after surgery, whether it’s arranging transportation or having someone help with daily tasks during your recovery period.
The Advantages of Minimally Invasive Surgery
Minimally invasive surgery has revolutionized how procedures are performed, offering patients faster recovery times and fewer complications. These techniques often involve smaller incisions, reduced scarring, and a quicker return to normal activities.
The Role of Regular Health Screenings
Screening is a cornerstone of preventive healthcare. Procedures like colonoscopies can detect issues such as polyps or colorectal cancer early, significantly improving treatment outcomes. Regular health check-ups and open communication with your healthcare provider are essential for staying proactive about your health.
Steps for a Quick Recovery
Recovering from surgery requires patience and adherence to your doctor’s recommendations. Here are some general tips to ensure a smooth recovery:
- Follow Discharge Instructions: Carefully read and follow the post-operative care guidelines provided by your surgeon.
- Stay Active (But Don’t Overdo It): Gentle movement, as recommended, can help prevent blood clots and improve healing.
- Eat a Balanced Diet: Proper nutrition supports your body’s recovery process, promoting faster healing.
Key Questions to Ask Before Hernia Repair Surgery
Before undergoing any surgical procedure, it’s important to have a thorough discussion with your surgeon. Key topics to cover include:
- The risks and benefits of the procedure.
- What to expect during the recovery period.
- Alternative treatments, if available.
Contact Us Today
Hernia repair is one of our specialties at Lenox Hill Minimally Invasive Surgery LLP. Call today to schedule your consultation with our expert surgeons.
LENOX HILL MINIALLY INVASIVE SURGERY LLP
155 East 76th Street
New York, NY 10021
Tel: 646-846-1136
Email: lenoxhillsurgeons@gmail.com
Post Surgery Recovery: Tips for a Smooth Healing Process
What are some good post surgery recovery tips? Recovering after surgery is just as important as the procedure itself. Whether you’ve undergone a minimally invasive laparoscopic operation or a more traditional open surgery, the healing process plays a vital role in ensuring optimal results and minimizing complications. While each individual and procedure may differ, there are universal strategies that can help support your recovery and enhance your overall well-being.

Follow Your Surgeon’s Instructions
Your post-operative instructions are tailored specifically to your surgery and individual health needs. These guidelines may include details on:
- Activity restrictions (e.g., lifting limits, walking requirements)
- Wound care and hygiene
- Medication usage
- Signs of infection or complications
Always follow these instructions closely and don’t hesitate to ask your care team for clarification if anything is unclear.
Pain Management Strategies
Managing pain effectively is essential for maintaining comfort and allowing you to move and heal. Most surgical pain improves gradually over time, but staying on top of it can prevent unnecessary stress and promote a smoother recovery.
- Take prescribed pain medications as directed
- Use ice packs or heating pads if recommended
- Practice deep breathing and relaxation techniques to reduce tension
- Discuss alternative pain relief options such as nerve blocks or over-the-counter medications with your doctor
Avoid waiting until the pain becomes unbearable. It’s more effective to manage pain preventively than to respond reactively.
Support Healing Through Nutrition
Your body requires energy and nutrients to rebuild tissue and fight off infection. A well-balanced diet can aid significantly in your healing process.
- Eat lean proteins like chicken, eggs, beans, and fish to support tissue repair
- Include fiber-rich foods to prevent post-surgical constipation
- Drink plenty of water to stay hydrated
- Limit sugar, alcohol, and processed foods
If you experience appetite loss or nausea, try eating small, frequent meals throughout the day.
Wound Care and Infection Prevention
Surgical site infections are one of the most common complications after surgery—but they’re largely preventable. Proper wound care helps reduce your risk and supports faster healing.
- Keep the surgical area clean and dry as instructed
- Do not remove surgical dressings or sutures unless directed
- Watch for signs of infection, such as redness, swelling, drainage, or fever
- Wash your hands thoroughly before touching the wound site
If you notice any signs of infection or unusual symptoms, contact your surgeon immediately.
Physical Activity and Gradual Mobility
While rest is important, so is movement. Early, gentle activity helps promote blood circulation, prevent blood clots, and reduce the risk of complications.
- Begin with short walks around the house or hospital
- Avoid strenuous activities, heavy lifting, and vigorous exercise until cleared
- Follow any prescribed physical therapy or stretching routines
- Listen to your body—don’t push through fatigue or sharp pain
Resuming normal activities gradually is key to building strength without risking injury.
Mental and Emotional Recovery
Surgery can be physically and emotionally taxing. Anxiety, fatigue, or even depression are common during recovery. Be kind to yourself and allow time for both physical and emotional healing.
- Stay connected with loved ones and accept help when offered
- Practice mindfulness, meditation, or journaling to reduce stress
- Talk to a mental health professional if feelings of sadness or anxiety persist
Healing is a holistic process, and your mental health plays a vital role in your physical recovery.
Know When to Call Your Doctor
While some discomfort is expected after surgery, certain symptoms warrant immediate medical attention. Contact your surgeon if you experience:
- Persistent or worsening pain
- Fever over 101°F (38.3°C)
- Excessive bleeding or wound discharge
- Difficulty breathing or chest pain
- Swelling in your legs or pain in the calf (a possible sign of a blood clot)
Early intervention can prevent minor issues from becoming serious problems.
Conclusion: Take an Active Role in Your Recovery
Recovery is a partnership between you and your surgical team. By staying informed, following recommendations, and listening to your body, you can set yourself up for a safe and successful healing process. Every step you take toward recovery matters—and with patience and consistency, you’ll be back to your routine feeling stronger than ever.
Need Guidance After Surgery?
If you’re preparing for surgery or currently recovering and want expert care every step of the way, the dedicated team at Lenox Hill Minimally Invasive Surgery PLLC is here for you. From advanced procedures to post-operative support, our mission is to help you heal with confidence.
LENOX HILL MINIMALLY INVASIVE SURGERY PLLC
Dr. Valery Dronsky
117 E 77th Street
New York, NY 10075
646-846-1136
admin@lenoxmis.com
How to Choose the Right Surgeon for Your Procedure
 How to choose the right surgeon for your procedure is one of the most important decisions you’ll make in your healthcare journey. Whether you’re facing a routine operation or a complex surgical intervention, your choice of surgeon can greatly impact the outcome, recovery, and overall experience. In a city like New York, where options are plentiful, knowing what to look for in a qualified and trustworthy surgeon is essential.
How to choose the right surgeon for your procedure is one of the most important decisions you’ll make in your healthcare journey. Whether you’re facing a routine operation or a complex surgical intervention, your choice of surgeon can greatly impact the outcome, recovery, and overall experience. In a city like New York, where options are plentiful, knowing what to look for in a qualified and trustworthy surgeon is essential.
Let’s walk through the key considerations for choosing the right surgeon, empowering you to make a confident and informed decision about your care.
Why Your Surgeon Choice Matters
The success of a surgical procedure is influenced not just by the procedure itself, but by the skill, experience, and approach of the surgeon performing it. The right surgeon can help you achieve:
- Optimal surgical outcomes with minimal complications
- A smoother, faster recovery
- Clear communication and peace of mind
- A personalized treatment plan tailored to your unique condition
On the other hand, choosing a surgeon who lacks specialization or experience in your particular procedure can increase risks and lead to a less satisfactory experience.
1. Verify Board Certification and Credentials
Start by confirming that the surgeon is board-certified by the American Board of Surgery or an appropriate specialty board. Board certification ensures the surgeon has completed extensive education and training and has passed rigorous exams.
Additionally, look for:
- Medical school and residency background
- Fellowship training in a subspecialty, if applicable
- Hospital affiliations (reputable institutions often have stricter credentialing)
2. Consider the Surgeon’s Experience with Your Procedure
Not all surgeons perform every type of surgery. Ideally, you want a specialist who performs your specific procedure regularly and has a proven track record of success.
Ask questions like:
- How many times have you performed this procedure?
- What are your success and complication rates?
- Have you treated patients with my specific condition?
Experience matters—surgeons who perform a high volume of specific procedures generally achieve better outcomes.
3. Evaluate the Use of Modern Techniques
The field of surgery continues to evolve, with many procedures now performed using minimally invasive or robotic techniques. These methods often result in:
- Smaller incisions
- Less postoperative pain
- Faster recovery times
- Reduced risk of infection
Ask if your procedure can be done using laparoscopic or robotic-assisted approaches and whether the surgeon is experienced with the latest technology.
4. Read Patient Reviews and Testimonials
Online reviews can provide insight into a surgeon’s bedside manner, communication skills, and the quality of their support team. While every practice may have a range of reviews, consistently positive feedback is a strong indicator of a patient-focused and skilled surgeon.
Look for reviews that mention:
- Patient satisfaction with outcomes
- Responsiveness to questions and concerns
- Clarity in explaining procedures and risks
5. Evaluate Communication and Comfort Level
Surgery can be a stressful experience. It’s important to feel comfortable with your surgeon and confident in their ability to guide you through the process. During your consultation, assess how well they:
- Listen to your concerns
- Explain procedures clearly and thoroughly
- Answer your questions without rushing
- Demonstrate empathy and professionalism
Your surgeon should be someone who values shared decision-making and includes you in the treatment planning process.
6. Understand the Practice’s Support and Follow-Up
A great surgical team includes more than just the surgeon. Consider the support offered by the practice, such as:
- Preoperative education and preparation
- Postoperative follow-up and care
- Access to nurses, physician assistants, and care coordinators
- Availability for questions and emergencies
The right team ensures continuity of care and a positive experience from start to finish.
7. Insurance and Logistics
While quality should never be compromised, make sure the surgeon accepts your insurance and that the associated hospitals or surgical centers are conveniently located and accredited.
Verify:
- Accepted insurance plans
- Availability of financing options, if needed
- Scheduling flexibility
Conclusion: Choose with Confidence
Choosing the right surgeon is a critical step toward a successful surgical outcome and a smoother recovery. By doing your research, asking the right questions, and trusting your instincts, you can feel confident in your decision. Take your time, explore your options, and never hesitate to seek a second opinion if needed.
If you’re in the New York City area and looking for expert surgical care delivered with compassion and precision, we welcome you to schedule a consultation with Dr. Valery Dronsky and the expert team at Lenox Hill Minimally Invasive Surgery.
Contact Information
LENOX HILL MINIMALLY INVASIVE SURGERY PLLC
Dr. Valery Dronsky
117 E 77th Street
New York, NY 10075
646-846-1136
admin@lenoxmis.com
Visit our website for more information:
https://www.lenoxhillminimallyinvasivesurgery.com
Advanced Techniques in Minimally Invasive Surgery
Here we’ll explore the most advanced techniques in minimally invasive surgery, their benefits, and how they’re being used to improve patient outcomes across a wide range of general surgical procedures. Minimally invasive surgery (MIS) has transformed modern medicine by offering patients safer procedures, shorter recovery times, and better cosmetic outcomes. As surgical technology evolves, so… Continue Reading
Why Lenox Hill Minimally Invasive Surgery PLLC is a Top Choice for NYC Patients
When selecting a surgical team in New York City, Lenox Hill Minimally Invasive Surgery PLLC, led by Dr. Valery Dronsky, provides experience, innovation, and compassionate care. The practice has earned its reputation as a trusted surgical practice by providing top-tier, patient-centered care using advanced minimally invasive techniques. For those seeking general surgery with less pain,… Continue Reading
The Importance of Regular Screenings and Early Detection
Regular screenings can lead to early detection and timely intervention for improving health outcomes and reducing mortality rates associated with serious medical conditions. Regular screenings play a crucial role in identifying diseases—particularly cancer and other chronic illnesses—at their earliest and most treatable stages. For patients in New York City and beyond, understanding the value of… Continue Reading
Understanding the Role of General Surgeons in Modern Healthcare
General surgeons play a vital and versatile role in the modern healthcare system. They are not only responsible for performing a wide range of surgical procedures but also serve as essential partners in the diagnosis, treatment, and post-operative care of many conditions. Unlike surgical specialists who focus on specific organs or systems, general surgeons are… Continue Reading
Preparing for Surgery: What Patients Need to Know
This guide covers essential steps and considerations when preparing for surgery, from preoperative consultations to post-surgical recovery. Undergoing surgery—whether minimally invasive or traditional—is a major medical event that requires preparation, both physically and mentally. Whether it’s a planned procedure like a hernia repair or an urgent appendectomy, knowing what to expect can help reduce anxiety… Continue Reading
Top Surgical Procedures Performed at Lenox Hill Minimally Invasive Surgery PLLC
Below is a comprehensive guide to the top general surgical procedures we perform, the conditions they treat, and what patients can expect. At Lenox Hill Minimally Invasive Surgery PLLC, our mission is to provide patients with safe, effective, and innovative surgical care using advanced minimally invasive techniques. Led by Dr. Valery Dronsky, our practice specializes… Continue Reading
Soft Tissue & Skin Surgery: Procedures for Lesions, Tumors, and Infections
This guide explores common soft tissue and skin conditions that may necessitate surgery, the types of surgical procedures used, and what patients can expect from the recovery process. The skin, the body’s largest organ, and soft tissues play a critical role in protecting us from infections, regulating body temperature, and enabling the sense of touch.… Continue Reading
Minimally Invasive Techniques in General Surgery: Advantages and Benefits
In this guide, we’ll explore what minimally invasive techniques in general surgery involves, the key advantages for patients, and the types of conditions commonly treated using these advanced methods. Minimally invasive surgery has transformed the field of general surgery, offering patients an effective way to address various health conditions with reduced pain, quicker recovery, and… Continue Reading
Spleen Surgery: Surgical Interventions for Splenic Conditions
In this guide, we’ll explore common splenic conditions that may require surgery, the types of surgical interventions available, and what patients can expect during recovery. The spleen is an important organ located in the upper left side of the abdomen. It plays a crucial role in filtering blood, fighting infections, and managing blood cells. Although… Continue Reading
General Surgery For Gastrointestinal Conditions
In this guide, we’ll explore common gastrointestinal conditions that may require surgery, the types of surgeries used to treat them, and the positive impact these procedures can have on patients’ lives. Gastrointestinal (GI) conditions encompass a wide range of disorders that affect the digestive system, including the stomach, intestines, liver, gallbladder, and pancreas. For many… Continue Reading
Small Intestine Surgery: Treatment Options for Intestinal Disorders
This comprehensive guide explores common small intestine disorders that may necessitate surgery, the types of surgical treatments available, and what patients can expect during the recovery process. The small intestine is a crucial part of the digestive system, responsible for absorbing nutrients from food and facilitating digestion. However, certain conditions and disorders can affect the… Continue Reading
General Surgery To Manage Chronic Pain?
Cqn general surgery be used to manage chronic pain? Having constant pain can significantly impact a person’s quality of life, affecting everything from mobility and sleep to mental health and daily functioning. While many individuals turn to medication, physical therapy, and other non-surgical options to manage pain, there are certain conditions where general surgery offers… Continue Reading